Carotid Sinus Hypersensitivity and Vasovagal Syncope are both conditions that can lead to temporary loss of consciousness. While they may share some similarities in symptoms, causes, and diagnostic approaches, it is important to understand the differences between these two conditions in order to provide appropriate treatment and management strategies. In this article, we will delve into the definition, causes, symptoms, diagnosis, and treatment options for both Carotid Sinus Hypersensitivity and Vasovagal Syncope, and highlight the implications for patient care.
Understanding Carotid Sinus Hypersensitivity
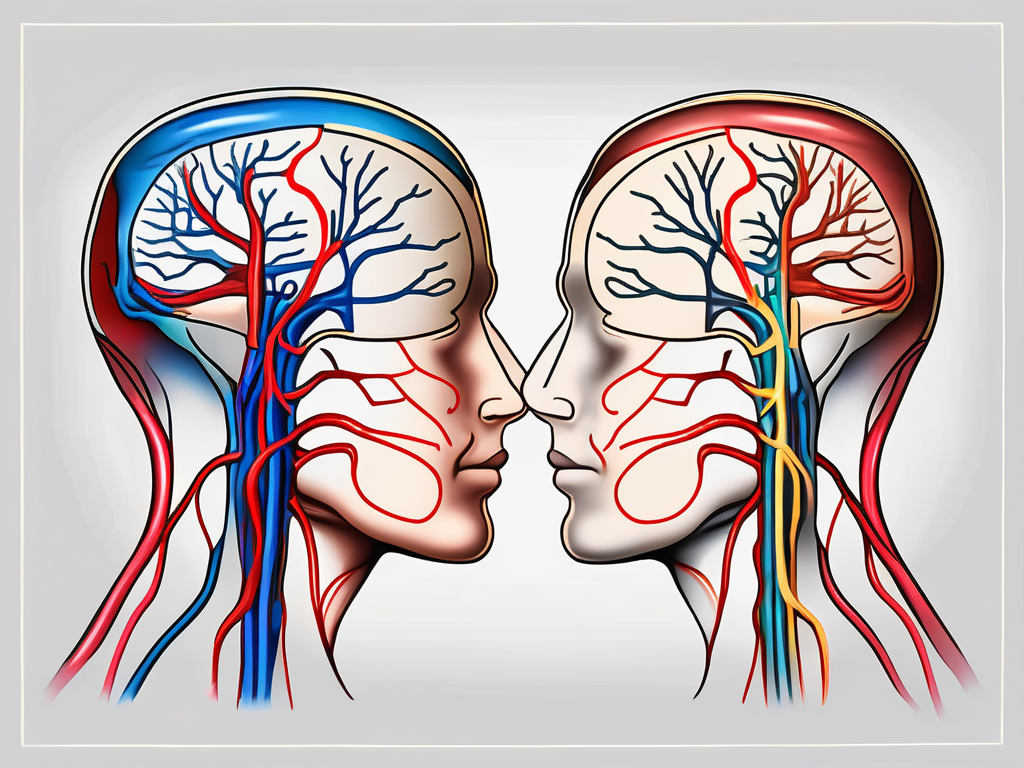
Carotid Sinus Hypersensitivity refers to an exaggerated response of the carotid sinus, a small area in the neck that contains baroreceptors responsible for regulating blood pressure. In individuals with carotid sinus hypersensitivity, the stimulation of the carotid sinus can lead to a sudden decrease in heart rate and blood pressure, resulting in loss of consciousness.
The exact causes of carotid sinus hypersensitivity are still not fully understood. However, it is believed that changes in the sensitivity of the baroreceptors or dysfunction of the autonomic nervous system may contribute to the development of this condition. Certain trigger factors, such as pressure on the carotid sinus during shaving or wearing tight collars, can also initiate the reflex response leading to syncope.
Carotid sinus hypersensitivity can affect individuals of all ages, although it is more commonly seen in older adults. It is also more prevalent in males than females. Understanding the underlying causes and risk factors associated with this condition is crucial in order to diagnose and manage it effectively.
Symptoms and Diagnosis of Carotid Sinus Hypersensitivity
The primary symptom of carotid sinus hypersensitivity is syncope, which is commonly referred to as fainting. In addition to syncope, individuals with carotid sinus hypersensitivity may experience dizziness, lightheadedness, or a feeling of impending collapse. It is important to note that these symptoms may also arise from other causes and do not necessarily indicate carotid sinus hypersensitivity.
When evaluating a patient for carotid sinus hypersensitivity, a thorough medical history is essential. The healthcare provider will inquire about the frequency and duration of syncopal episodes, as well as any triggering factors. A physical examination will also be conducted to assess the patient’s overall health and to rule out other potential causes of syncope.
In addition to the medical history and physical examination, specific tests can help in diagnosing carotid sinus hypersensitivity. These tests may include a carotid sinus massage, along with electrocardiogram monitoring, blood pressure measurements, and echocardiography. The carotid sinus massage involves applying gentle pressure to the carotid sinus to assess the response of the baroreceptors. This procedure is typically performed in a controlled setting under the supervision of a healthcare professional.
Diagnosing carotid sinus hypersensitivity can be challenging, as the symptoms are often nonspecific and can overlap with other conditions. Therefore, a comprehensive evaluation is necessary to differentiate carotid sinus hypersensitivity from other causes of syncope.
Treatment Options for Carotid Sinus Hypersensitivity
The treatment approach for carotid sinus hypersensitivity depends on the severity of symptoms and individual patient factors. In milder cases, lifestyle modifications may be recommended as the first line of treatment. These modifications may include avoiding triggering factors, increasing fluid and salt intake, and wearing compression stockings. These lifestyle changes aim to improve blood circulation and minimize the risk of syncopal episodes.
In more severe cases of carotid sinus hypersensitivity, medications may be prescribed to prevent syncopal episodes. Beta-blockers, which help regulate heart rate and blood pressure, are commonly used in the management of this condition. Anticholinergic agents, which block certain nerve signals, may also be prescribed to reduce the sensitivity of the carotid sinus.
In certain cases, surgical interventions may be considered for individuals with severe and refractory carotid sinus hypersensitivity. Carotid sinus denervation involves surgically interrupting the nerve pathways responsible for the exaggerated response of the carotid sinus. Pacemaker implantation, on the other hand, aims to regulate heart rate and prevent sudden drops in blood pressure. These interventions should only be pursued after careful evaluation and consultation with a qualified healthcare professional.
It is important for individuals with carotid sinus hypersensitivity to work closely with their healthcare team to develop an individualized treatment plan. Regular follow-up appointments and ongoing monitoring are essential to ensure the effectiveness of the chosen treatment approach and to make any necessary adjustments.
Exploring Vasovagal Syncope
Vasovagal syncope is a fascinating condition that affects many individuals worldwide. It is characterized by a sudden drop in heart rate and blood pressure, leading to a temporary loss of consciousness. This reflex syncope occurs due to an overactive vagus nerve, which causes the dilation of blood vessels and a decrease in heart rate.
While the exact causes of vasovagal syncope can vary from person to person, there are several common triggers that have been identified. Emotional stress, such as anxiety or fear, can often lead to a syncopal episode. Intense pain, whether it be from an injury or a medical procedure, can also trigger vasovagal syncope. Prolonged standing, particularly in hot and crowded environments, can cause blood to pool in the legs and result in a sudden drop in blood pressure. Dehydration is another common trigger, as it can lead to a decrease in blood volume and subsequent syncope.
It is important to note that certain medications and medical conditions can increase the risk of vasovagal syncope. Individuals with structural heart disease or autonomic dysfunction are more prone to experiencing syncopal episodes. Medications that affect blood pressure or heart rate, such as beta-blockers or certain antidepressants, can also contribute to the development of vasovagal syncope.
Recognizing the symptoms of vasovagal syncope is crucial for early intervention. Dizziness and lightheadedness are often the first signs that an individual may experience a syncopal episode. Nausea and sweating may also accompany these symptoms. In some cases, individuals may notice visual changes, such as blurred vision or tunnel vision, before losing consciousness. It is important to note that these symptoms typically subside once the individual assumes a lying or sitting position, as blood flow to the brain is restored.
Treatment and management of vasovagal syncope primarily focus on identifying and addressing the underlying triggers or contributors. Lifestyle modifications can play a significant role in preventing syncopal episodes. Increasing fluid and salt intake can help maintain adequate blood volume and prevent dehydration. Regular exercise, particularly exercises that promote blood circulation, can also be beneficial. It is important for individuals to be aware of their triggers and avoid situations that may lead to syncope.
In severe cases, medications may be prescribed to reduce the frequency and severity of syncope episodes. Beta-blockers, which help regulate heart rate and blood pressure, are commonly used. Selective serotonin reuptake inhibitors (SSRIs), typically prescribed for depression and anxiety, have also shown some effectiveness in managing vasovagal syncope. Additionally, physical counterpressure maneuvers can be used to abort an imminent syncopal episode. Crossing the legs, tensing the muscles, or performing other similar actions can help increase blood flow to the brain and prevent loss of consciousness.
Vasovagal syncope is a complex condition that requires individualized management. By understanding the causes, symptoms, and treatment options, individuals can take proactive steps to prevent syncopal episodes and improve their quality of life.
Comparing Carotid Sinus Hypersensitivity and Vasovagal Syncope
Similarities in Symptoms and Diagnosis
Carotid sinus hypersensitivity and vasovagal syncope both present with similar symptoms, including syncope, dizziness, and lightheadedness. Syncope, commonly known as fainting, is a temporary loss of consciousness caused by a sudden drop in blood flow to the brain. This can be accompanied by a feeling of lightheadedness or dizziness, making it difficult for individuals to maintain their balance.
When it comes to diagnosis, healthcare professionals follow a similar approach for both conditions. They begin by taking a thorough medical history, which includes asking about the frequency and duration of syncopal episodes, as well as any potential triggers. A physical examination is then conducted to check for any underlying medical conditions or abnormalities that may contribute to the symptoms.
In addition to the medical history and physical examination, specific tests are performed to rule out other potential causes of the symptoms. These tests may include an electrocardiogram (ECG) to evaluate the heart’s electrical activity, an echocardiogram to assess the structure and function of the heart, and a tilt table test to provoke and evaluate the response to certain triggers.
Differences in Causes and Risk Factors
While both conditions involve an exaggerated reflex response leading to syncope, the underlying causes and risk factors differ. Carotid sinus hypersensitivity is primarily associated with dysfunction of the carotid sinus and the autonomic nervous system. The carotid sinus, located in the neck, is responsible for regulating blood pressure and heart rate. Dysfunction in this area can lead to an overactive response, causing a sudden drop in blood pressure and subsequent syncope.
On the other hand, vasovagal syncope is often triggered by emotional stress, pain, or dehydration. The vagus nerve, which plays a crucial role in regulating heart rate and blood pressure, becomes overstimulated in response to certain triggers. This overstimulation leads to a sudden decrease in heart rate and blood pressure, resulting in syncope.
Furthermore, there are differences in the risk factors associated with each condition. Carotid sinus hypersensitivity is more common in older individuals, especially those with a history of cardiovascular disease. Other risk factors include carotid artery disease, recent neck surgery, and certain medications that affect blood pressure. In contrast, vasovagal syncope is more prevalent in younger individuals, particularly during adolescence and early adulthood. Emotional stress, prolonged standing, and certain medications are common triggers for vasovagal syncope.
Treatment Approaches: A Comparative Analysis
The treatment approaches for carotid sinus hypersensitivity and vasovagal syncope also differ based on the underlying causes and severity of symptoms. Carotid sinus hypersensitivity may require lifestyle modifications, medications, or surgical interventions. Lifestyle modifications often include avoiding triggers such as sudden neck movements or tight collars. Medications such as beta-blockers or calcium channel blockers may be prescribed to help regulate heart rate and blood pressure. In severe cases, surgical interventions such as carotid sinus massage or carotid sinus denervation may be considered.
On the other hand, the management of vasovagal syncope mainly focuses on identifying triggers and utilizing lifestyle modifications and medications to prevent syncopal episodes. Lifestyle modifications may involve maintaining adequate hydration, avoiding prolonged standing, and learning techniques to manage emotional stress. Medications such as beta-blockers or selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help regulate heart rate and blood pressure, as well as reduce the frequency and severity of syncopal episodes.
In some cases, if lifestyle modifications and medications are not effective, other treatment options such as pacemakers or implantable loop recorders may be considered to monitor and regulate heart rhythm.
Implications for Patient Care
The implications for patient care in the context of syncope are vast and multifaceted. Syncope, a temporary loss of consciousness caused by a sudden drop in blood flow to the brain, can have various underlying causes. These causes can range from benign conditions such as vasovagal syncope to more serious conditions like carotid sinus hypersensitivity. As a result, tailoring treatment to the individual becomes paramount in ensuring effective management and optimal patient outcomes.
Tailoring Treatment to the Individual
Due to the differences in causes and treatment approaches, it is essential to tailor the treatment plan for each individual, considering their specific condition and symptoms. This personalized approach ensures that patients receive the most appropriate care based on their unique circumstances. Consulting with a healthcare professional who specializes in syncope is highly recommended to ensure an accurate diagnosis and appropriate treatment.
When tailoring treatment to the individual, healthcare professionals take into account various factors such as the patient’s medical history, age, lifestyle, and any underlying medical conditions. This comprehensive evaluation helps determine the most suitable treatment options, which may include lifestyle modifications, medication management, or even surgical interventions in certain cases.
The Importance of Accurate Diagnosis
Accurate diagnosis is crucial for determining the appropriate management strategies for individuals experiencing syncope. A comprehensive evaluation, including a detailed history, physical examination, and diagnostic tests, can help differentiate between carotid sinus hypersensitivity and vasovagal syncope, and guide treatment decisions.
During the diagnostic process, healthcare professionals may employ various tests such as electrocardiograms (ECGs), echocardiograms, tilt table tests, and carotid sinus massage. These tests provide valuable insights into the underlying cause of syncope and aid in formulating an accurate diagnosis.
It is worth noting that accurate diagnosis not only helps in determining the most appropriate treatment plan but also plays a crucial role in ruling out any potentially life-threatening conditions that may present with syncope-like symptoms. This underscores the importance of seeking medical advice and consultation with a healthcare professional experienced in the management of syncope.
Long-term Management and Prognosis
Long-term management of both carotid sinus hypersensitivity and vasovagal syncope focuses on minimizing the risk of syncopal episodes and improving the quality of life for affected individuals. This management approach involves a combination of strategies aimed at preventing syncope, addressing underlying causes, and providing support to patients.
Regular follow-up visits with healthcare professionals are crucial in monitoring the effectiveness of treatment plans and making any necessary adjustments. These visits also serve as an opportunity for patients to discuss any concerns or new symptoms they may be experiencing.
In addition to medical interventions, lifestyle modifications can play a significant role in long-term management. These modifications may include increasing fluid and salt intake, avoiding triggers that can induce syncope, and maintaining a regular sleep schedule. Engaging in regular physical activity, when appropriate, can also help improve cardiovascular health and reduce the frequency of syncopal episodes.
Adherence to treatment plans is vital for successful long-term management. Patients are encouraged to take medications as prescribed, follow recommended dietary and lifestyle modifications, and promptly report any changes in symptoms to their healthcare providers.
While the prognosis for individuals with syncope varies depending on the underlying cause and individual factors, early diagnosis and appropriate management can significantly improve outcomes. By effectively managing syncope, the risk of complications and the impact on daily life can be minimized.
In conclusion, while carotid sinus hypersensitivity and vasovagal syncope have some similarities in their symptoms and diagnostic approaches, they have distinct causes and treatment strategies. It is crucial to differentiate between these conditions to provide appropriate care and improve patient outcomes. If you or someone you know experiences syncope or related symptoms, it is recommended to seek medical advice and consultation with a healthcare professional experienced in the management of these conditions.







Leave a Reply