Vasovagal syncope and orthostatic hypotension are two conditions that often cause similar symptoms, but they have distinct differences in their underlying mechanisms and treatment approaches. Understanding these differences is crucial for proper diagnosis and appropriate management. In this article, we will delve into the intricacies of vasovagal syncope and orthostatic hypotension, exploring their physiology, triggers, symptoms, diagnosis methods, and treatment options. By the end, you will have a clear understanding of how these conditions differ and the steps you can take to alleviate their impact on your daily life.
Defining Vasovagal Syncope
Vasovagal syncope, also known as neurocardiogenic syncope or reflex syncope, is a condition characterized by a sudden loss of consciousness due to a temporary drop in blood pressure and heart rate. It commonly occurs in response to certain triggers, such as emotional stress, pain, dehydration, prolonged standing, or even the sight of blood. While vasovagal syncope can affect individuals of any age, it is more prevalent among young adults.
The Physiology Behind Vasovagal Syncope
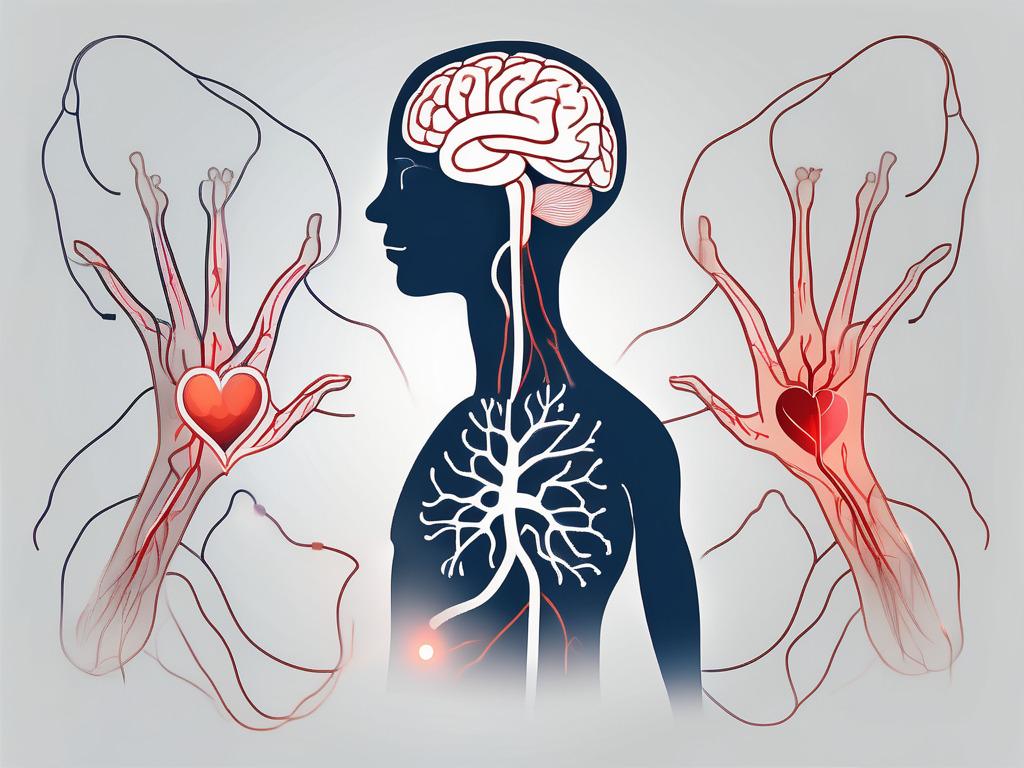
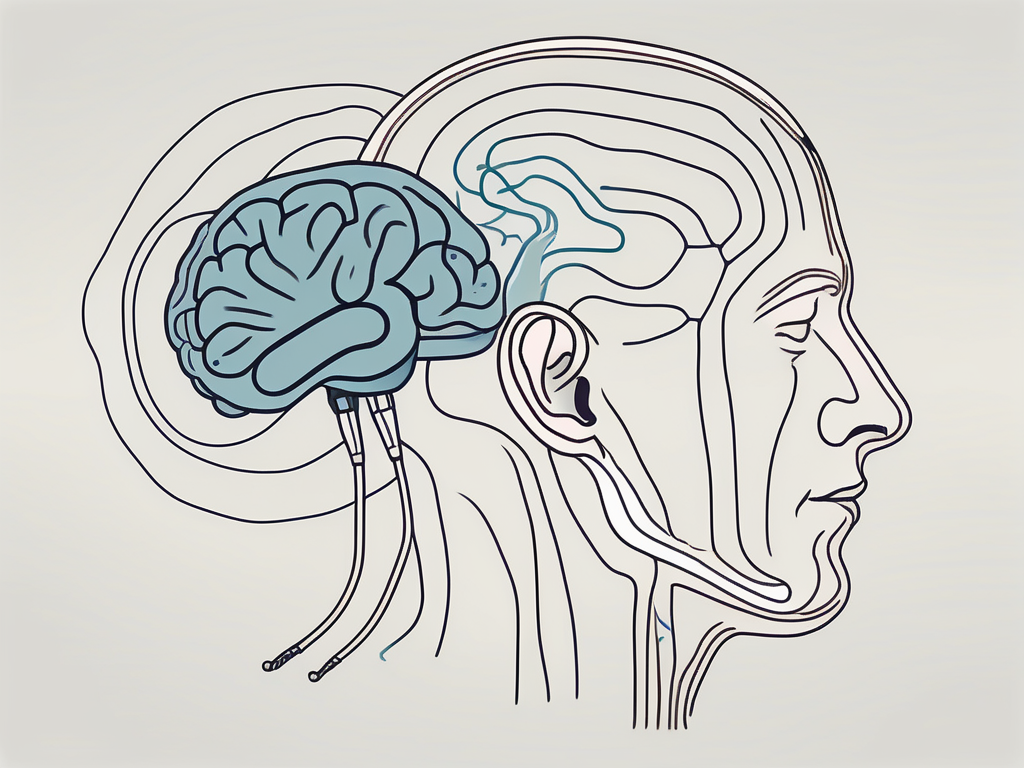
Vasovagal syncope involves a complex interplay of the nervous system, particularly the vagus nerve, and the cardiovascular system. When triggered, the parasympathetic nervous system becomes activated, resulting in a decrease in heart rate and the dilation of blood vessels, which collectively lead to a reduction in blood pressure. In some cases, this response becomes exaggerated, causing a sudden decrease in cerebral blood flow and resulting in loss of consciousness.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, and digestion. It consists of both sensory and motor fibers that innervate organs in the chest, abdomen, and neck. When the vagus nerve is stimulated, it releases neurotransmitters that modulate the activity of the heart and blood vessels.
During a vasovagal syncope episode, the vagus nerve becomes overstimulated, leading to a cascade of physiological changes. The heart rate slows down, reducing the amount of blood pumped out with each heartbeat. At the same time, the blood vessels dilate, causing blood to pool in the lower extremities. These combined effects result in a sudden drop in blood pressure, depriving the brain of oxygen and nutrients, ultimately leading to loss of consciousness.
Common Triggers of Vasovagal Syncope
Vasovagal syncope can be precipitated by a variety of triggers, which can vary from person to person. Emotional stress, such as anxiety or fear, is a common trigger. The body’s response to stress involves the release of stress hormones, which can activate the vagus nerve and trigger a vasovagal episode.
Prolonged standing can also lead to vasovagal syncope, especially when combined with factors such as heat exposure or dehydration. When standing for extended periods, blood can pool in the lower extremities, reducing the amount of blood available to the brain. Dehydration further exacerbates this effect by decreasing blood volume and compromising the body’s ability to maintain blood pressure.
Other triggers of vasovagal syncope include sudden changes in posture, such as standing up quickly from a seated or lying position. This rapid change in position can cause a sudden drop in blood pressure, leading to a vasovagal episode. Pain, whether acute or chronic, can also activate the vagus nerve and trigger syncope in susceptible individuals.
Additionally, certain medical procedures, such as blood draws or injections, can act as triggers for vasovagal syncope. The sight of blood or the anticipation of a medical procedure can induce anxiety or fear, activating the body’s stress response and potentially leading to a vasovagal episode.
Symptoms and Diagnosis of Vasovagal Syncope
The symptoms of vasovagal syncope typically include lightheadedness, dizziness, nausea, blurred vision, and a sudden loss of consciousness. These symptoms are usually short-lived, lasting only a few seconds to a few minutes. However, the impact on daily life can be significant, leading to limitations in activities and a fear of recurrent episodes.
Diagnosing vasovagal syncope involves a detailed medical history, physical examination, and various tests to rule out other causes of fainting. Your healthcare provider may also recommend diagnostic tools such as an electrocardiogram (ECG) or a tilt-table test to assess your autonomic nervous system’s response to changes in posture.
An ECG measures the electrical activity of the heart and can help identify any underlying heart rhythm abnormalities that may contribute to syncope. A tilt-table test involves lying on a table that is tilted to different angles while being closely monitored. This test helps evaluate how your body responds to changes in position and can help confirm a diagnosis of vasovagal syncope.
It is important to note that while vasovagal syncope can be disruptive and distressing, it is generally not life-threatening. However, if you experience recurrent episodes of syncope or have concerns about your symptoms, it is essential to seek medical evaluation and guidance for proper management.
Exploring Orthostatic Hypotension
Orthostatic hypotension, sometimes referred to as postural hypotension, is a condition characterized by a sudden drop in blood pressure upon standing up or changing positions. This drop in blood pressure can cause dizziness, lightheadedness, and, in severe cases, fainting. Orthostatic hypotension is more common among older adults, although it can occur at any age.
The Science of Orthostatic Hypotension
The underlying mechanism of orthostatic hypotension involves an impaired ability of the autonomic nervous system to regulate blood pressure appropriately. When we stand up, gravity causes a slight redistribution of blood in our bodies, with more blood pooling in the lower extremities. Normally, the autonomic nervous system triggers certain compensation mechanisms, such as increasing heart rate and narrowing blood vessels, to maintain blood pressure. However, in individuals with orthostatic hypotension, these compensatory responses may be inadequate, resulting in a drop in blood pressure and associated symptoms.
Furthermore, research has shown that orthostatic hypotension can also be influenced by factors such as age and gender. Older adults are more prone to experiencing orthostatic hypotension due to age-related changes in blood vessels and the autonomic nervous system. Additionally, studies have found that women may be more susceptible to orthostatic hypotension compared to men, although the reasons for this gender difference are not yet fully understood.
Causes and Risk Factors for Orthostatic Hypotension
Orthostatic hypotension can be caused by various factors, including certain medications, dehydration, prolonged bed rest, and autonomic nervous system disorders such as Parkinson’s disease. Additionally, conditions that affect blood volume and circulation, such as heart disease and diabetes, can increase the risk of developing orthostatic hypotension. Identifying and addressing the underlying cause is crucial for effective management.
It is important to note that some medications commonly prescribed for other conditions, such as high blood pressure or heart disease, can actually contribute to the development of orthostatic hypotension. These medications may interfere with the body’s ability to regulate blood pressure, making individuals more susceptible to experiencing drops in blood pressure upon standing or changing positions. Therefore, healthcare providers must carefully consider the potential side effects of medications when assessing and managing orthostatic hypotension.
Identifying Symptoms and Diagnostic Methods for Orthostatic Hypotension
The symptoms of orthostatic hypotension typically include dizziness, lightheadedness, blurred vision, and even fainting upon standing or changing positions. These symptoms may resolve quickly once the person lies down or sits for a while. Diagnosing orthostatic hypotension often involves measuring blood pressure in different positions, such as lying down, sitting, and standing, to detect significant drops upon posture changes. Your healthcare provider may also recommend additional tests to evaluate potential underlying causes.
Moreover, it is important to differentiate orthostatic hypotension from other conditions that may present with similar symptoms. For example, conditions like vertigo or inner ear disorders can also cause dizziness and lightheadedness. Therefore, a comprehensive evaluation by a healthcare professional is necessary to accurately diagnose orthostatic hypotension and determine the appropriate treatment plan.
In conclusion, orthostatic hypotension is a complex condition that involves the autonomic nervous system’s ability to regulate blood pressure. Various factors, including age, gender, medications, and underlying health conditions, can contribute to the development of orthostatic hypotension. Recognizing the symptoms and obtaining an accurate diagnosis are crucial for effective management and improving quality of life for individuals with this condition.
Comparing Vasovagal and Orthostatic Conditions
While vasovagal syncope and orthostatic hypotension share similarities in terms of symptoms, such as dizziness and fainting, there are some key differences between the two conditions.
Vasovagal syncope and orthostatic hypotension are both medical conditions that can cause a sudden drop in blood pressure, leading to similar symptoms. When blood pressure drops significantly, it can result in dizziness, lightheadedness, and even fainting. These symptoms can be quite alarming and can greatly impact an individual’s quality of life.
Additionally, both vasovagal syncope and orthostatic hypotension can be triggered by various factors. Dehydration, for example, can contribute to the development of both conditions. When the body lacks adequate fluid, it can affect blood volume and subsequently lead to a drop in blood pressure. Prolonged standing can also be a trigger for both conditions. When a person stands for an extended period, blood can pool in the lower extremities, causing a decrease in blood flow to the brain and resulting in symptoms such as dizziness and fainting. Furthermore, sudden changes in posture, such as quickly standing up from a seated or lying position, can provoke both vasovagal syncope and orthostatic hypotension.
Key Differences between Vasovagal Syncope and Orthostatic Hypotension
Despite certain commonalities, vasovagal syncope and orthostatic hypotension are distinct conditions with different underlying mechanisms.
Vasovagal syncope is primarily mediated by the vagus nerve and involves an exaggerated parasympathetic response. The vagus nerve plays a crucial role in regulating heart rate and blood pressure. In individuals with vasovagal syncope, certain triggers can stimulate the vagus nerve, leading to a sudden drop in blood pressure and a decrease in heart rate. This response is often accompanied by symptoms such as lightheadedness, nausea, and even temporary loss of consciousness.
On the other hand, orthostatic hypotension stems from an impaired autonomic nervous system’s ability to regulate blood pressure adequately. The autonomic nervous system is responsible for maintaining blood pressure within a normal range, regardless of body position. In individuals with orthostatic hypotension, the body struggles to adjust blood pressure appropriately when changing positions, such as standing up. This can result in a sudden drop in blood pressure, leading to symptoms similar to vasovagal syncope.
In terms of treatment approaches, vasovagal syncope often requires lifestyle modifications, such as increasing fluid intake and avoiding triggers. Staying well-hydrated can help maintain blood volume and prevent sudden drops in blood pressure. Identifying and avoiding triggers, such as prolonged standing or emotional stress, can also be beneficial in managing vasovagal syncope.
On the other hand, orthostatic hypotension may necessitate medications or interventions that help maintain blood pressure upon position changes. Medications such as fludrocortisone can be prescribed to increase blood volume and improve blood pressure regulation. Additionally, wearing compression stockings can help prevent blood pooling in the lower extremities, reducing the risk of orthostatic hypotension symptoms.
In conclusion, while vasovagal syncope and orthostatic hypotension share similarities in terms of symptoms and triggers, they have different underlying mechanisms and may require different treatment approaches. Understanding these differences can aid in accurate diagnosis and appropriate management of these conditions.
Treatment and Management Strategies
Treating Vasovagal Syncope
When it comes to treating vasovagal syncope, the primary focus is on identifying and avoiding triggers. Vasovagal syncope is often triggered by certain situations or stimuli, such as standing for long periods, seeing blood, or experiencing extreme emotional distress. By recognizing these triggers, you can take proactive steps to prevent syncope episodes.
Maintaining good hydration is crucial in managing vasovagal syncope. Dehydration can exacerbate symptoms and increase the risk of fainting. This is especially important during hot weather or periods of increased physical activity when the body loses more fluids through sweating.
If anxiety or stress plays a role in your episodes, stress reduction techniques and relaxation exercises may be beneficial. These can help calm your mind and body, reducing the likelihood of a vasovagal response.
In some cases, your healthcare provider may prescribe medications that help stabilize blood pressure and heart rate. These medications can be used to prevent syncope episodes or reduce their severity. It is important to discuss the potential benefits and risks of medication with your healthcare provider.
It is important to note that the management of vasovagal syncope should be individualized. Each person may have different triggers and require a tailored treatment plan. Consulting with your healthcare provider is essential for developing an appropriate treatment plan that addresses your specific needs.
Managing Orthostatic Hypotension
The management of orthostatic hypotension often involves addressing the underlying cause, if possible. Orthostatic hypotension can be caused by various factors, including medication side effects, dehydration, and certain medical conditions. Identifying and treating the root cause can help alleviate symptoms.
In cases where medication side effects contribute to orthostatic hypotension, adjusting medication dosages or switching to alternative medications may be necessary. It is important to work closely with your healthcare provider to find the right balance between managing your condition and minimizing medication-related side effects.
Lifestyle adjustments can also play a significant role in managing orthostatic hypotension. Increasing fluid and salt intake can help expand blood volume and raise blood pressure. Wearing compression stockings can improve blood flow and prevent blood pooling in the legs. Regularly performing leg exercises, such as ankle pumps and calf raises, can help improve muscle tone and reduce the risk of dizziness upon standing.
In more severe cases of orthostatic hypotension, your healthcare provider may recommend medications that help raise blood pressure. These medications work by constricting blood vessels or increasing blood volume, thereby improving blood flow and reducing the risk of fainting.
Given the complex nature of orthostatic hypotension, it is crucial to work closely with your healthcare provider to identify the most appropriate treatment options based on your specific situation. Regular follow-up appointments and open communication with your healthcare team are essential for managing your condition effectively.
Prevention and Lifestyle Adjustments
Lifestyle Changes for Vasovagal Syncope
For individuals with vasovagal syncope, making certain lifestyle adjustments can be beneficial in minimizing the frequency and severity of episodes. Staying well-hydrated, particularly in warm environments or during physical activity, can help prevent blood pressure drops. Regular exercise, especially exercises that involve changing positions, may also help improve blood circulation and reduce the risk of syncope. Additionally, stress management techniques, such as deep breathing exercises or mindfulness practices, can help reduce anxiety levels and potentially prevent vasovagal episodes.
It is important to remember that lifestyle changes should be implemented under the guidance of a healthcare professional. Consulting with a doctor and working together to develop a tailored plan is essential.
Preventive Measures for Orthostatic Hypotension
To prevent or manage orthostatic hypotension, there are several measures you can take. Increasing fluid and salt intake can help increase blood volume and maintain blood pressure. Daily exercise, particularly activities that promote leg muscle contraction, can improve blood circulation and minimize blood pooling in the lower extremities. Wearing compression stockings or abdominal binders may also be beneficial in preventing blood from pooling and minimizing blood pressure drops.
It is essential to note that preventive measures should be discussed with a healthcare provider to ensure they are suitable for your specific case.
In Conclusion
Vasovagal syncope and orthostatic hypotension, while sharing similar symptoms, are distinct conditions with different underlying mechanisms and treatment approaches. Understanding the differences between these conditions is crucial for appropriate diagnosis and management. Remember, if you experience recurrent or severe episodes of dizziness, lightheadedness, or fainting, it is important to consult with a healthcare professional for an accurate diagnosis and proper guidance. With their expertise and your commitment to a proactive approach, you can navigate these conditions and minimize their impact on your day-to-day life.




Leave a Reply