Vasovagal syncope, also known as neurocardiogenic syncope, is a condition characterized by a sudden loss of consciousness due to a temporary decrease in blood flow to the brain. In some cases, vasovagal syncope can be accompanied by convulsions, which are involuntary muscle contractions. This article aims to provide an in-depth understanding of vasovagal syncope with convulsions, including its causes, symptoms, diagnostic procedures, treatment options, and preventive measures. Please note that the information provided in this article is for educational purposes only, and it is essential to consult with a healthcare professional for proper diagnosis and treatment.
What is Vasovagal Syncope?
Vasovagal syncope is a type of fainting episode that occurs when the body overreacts to certain triggers, resulting in a sudden drop in blood pressure and heart rate. This, in turn, reduces blood flow to the brain, leading to a loss of consciousness. While fainting is relatively common and often harmless, it is essential to understand the underlying causes of vasovagal syncope, especially when accompanied by convulsions.
Definition and Overview of Vasovagal Syncope
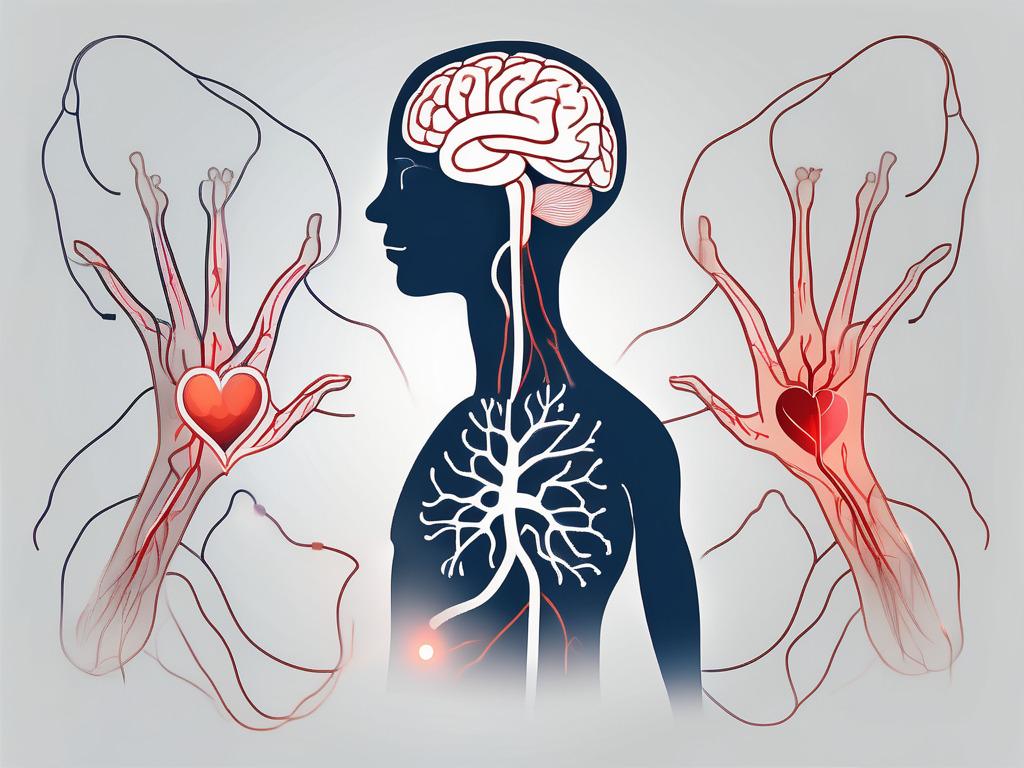
Vasovagal syncope is a reflex-mediated response that involves the interaction between the autonomic nervous system and the cardiovascular system. When a triggering event occurs, such as seeing blood, experiencing emotional distress, or standing up too quickly, the body responds with a sudden drop in blood pressure and heart rate, causing the individual to faint momentarily. Vasovagal syncope can occur in individuals of any age, although it is more common in teenagers and young adults.
When a person experiences vasovagal syncope, several physiological changes occur in their body. The autonomic nervous system, which regulates involuntary bodily functions, becomes overactive, leading to a rapid decrease in blood pressure. Additionally, the heart rate slows down significantly, reducing the amount of blood pumped to the brain. As a result, the brain does not receive enough oxygen and nutrients, leading to a loss of consciousness.
It is important to note that vasovagal syncope is a temporary condition and typically resolves on its own. However, recurrent episodes of syncope should be evaluated by a healthcare professional to rule out any underlying medical conditions.
The Connection Between Vasovagal Syncope and Convulsions
In some cases, individuals with vasovagal syncope may experience convulsions, or involuntary muscle contractions, during the fainting episode. These convulsions can last for a few seconds to a few minutes and are typically self-limiting. The exact mechanism behind the occurrence of convulsions during vasovagal syncope is not well understood, but it may be related to the brain’s response to the temporary lack of oxygen and blood flow.
Convulsions, also known as seizures, are abnormal electrical activities in the brain that result in uncontrolled movements and changes in behavior. They can manifest as jerking or twitching of the limbs, loss of muscle tone, or even loss of consciousness. While convulsions during vasovagal syncope may be alarming, they are generally not indicative of a more severe underlying condition.
During a vasovagal syncope episode, the brain temporarily loses its normal blood supply, leading to a disruption in its normal functioning. This lack of oxygen and nutrients can trigger abnormal electrical discharges in the brain, resulting in convulsions. However, it is essential to differentiate between vasovagal syncope-related convulsions and seizures caused by other medical conditions, as the treatment approaches may vary.
If an individual experiences convulsions during a vasovagal syncope episode, it is crucial to ensure their safety by gently guiding them to the ground and removing any objects that may cause injury. Once the convulsions subside, the person usually regains consciousness and may feel weak or disoriented. It is advisable to seek medical attention to evaluate the underlying cause of the syncope episode and determine appropriate management strategies.
Causes of Vasovagal Syncope with Convulsions
Understanding the causes of vasovagal syncope with convulsions is crucial in managing and preventing these episodes adequately. While the exact triggers may vary from individual to individual, several factors contribute to the development of vasovagal syncope:
Biological Factors Leading to Vasovagal Syncope
Various biological factors can increase the likelihood of experiencing vasovagal syncope. One such factor is an overactive response of the autonomic nervous system, which controls involuntary bodily functions. When this response is exaggerated, it can lead to a sudden drop in blood pressure and heart rate, resulting in syncope. Additionally, certain genetic predispositions can make individuals more susceptible to vasovagal syncope with convulsions. Researchers have identified specific gene variants that are associated with an increased risk of experiencing syncope episodes. Furthermore, underlying medical conditions such as heart disease or blood pressure disorders can also contribute to the development of vasovagal syncope. These conditions can disrupt the normal functioning of the cardiovascular system, making individuals more prone to experiencing syncope episodes. However, it is important to note that vasovagal syncope with convulsions can occur in individuals without any underlying health conditions, highlighting the complex nature of this condition.
Environmental Triggers for Vasovagal Syncope and Convulsions
Environmental factors play a significant role in triggering vasovagal syncope episodes, often in combination with biological factors. Sudden emotional stress, such as receiving distressing news or experiencing a traumatic event, can activate the body’s fight-or-flight response, leading to a cascade of physiological changes that can result in syncope. Similarly, intense pain can trigger a vasovagal response, causing a drop in blood pressure and subsequent loss of consciousness. Prolonged standing or being in an upright position for an extended period can also contribute to the development of vasovagal syncope. When standing, blood can pool in the lower extremities, leading to decreased blood flow to the brain and potential syncope. Exposure to extreme temperatures, both hot and cold, can also trigger vasovagal syncope. In hot environments, the body may struggle to dissipate heat, leading to dehydration and a subsequent drop in blood pressure. Cold temperatures can cause blood vessels to constrict, reducing blood flow and potentially triggering syncope. Additionally, dehydration, whether due to inadequate fluid intake or excessive fluid loss, can increase the risk of vasovagal syncope. Finally, certain medications, such as those used to treat high blood pressure or anxiety, can have side effects that contribute to syncope episodes. Identifying and avoiding these triggers can be helpful in managing vasovagal syncope and reducing the chances of convulsions occurring during an episode.
Recognizing the Symptoms of Vasovagal Syncope and Convulsions
Recognizing the symptoms of vasovagal syncope and convulsions is crucial in seeking appropriate medical attention and finding ways to manage and prevent future episodes. The symptoms may vary from individual to individual, and they can be categorized into two main groups:
Physical Signs and Symptoms
Physical signs and symptoms of vasovagal syncope include dizziness, lightheadedness, blurred vision, nausea, sweating, pale skin, and a rapid, weak pulse. These symptoms can occur shortly before a fainting episode and may be followed by convulsions in some cases.
When experiencing vasovagal syncope, individuals may feel a sudden wave of dizziness, making it difficult to maintain balance and causing the world around them to spin. Lightheadedness can intensify, leading to a feeling of impending faintness. Vision becomes blurry, making it challenging to focus on objects or read text. Nausea may arise, accompanied by an uncomfortable sensation in the stomach. Sweat beads may form on the forehead and body, as the body attempts to regulate its temperature. The skin may lose its natural color, becoming pale and clammy. The pulse may become rapid and weak, reflecting the body’s struggle to maintain blood flow.
It is important to note that convulsions during vasovagal syncope are usually self-limiting and do not require emergency medical attention. However, if the convulsions are prolonged or accompanied by other concerning symptoms, immediate medical assistance should be sought.
Emotional and Psychological Indicators
Emotional and psychological indicators of vasovagal syncope are often experienced both during and after an episode. These can include anxiety, fear, confusion, and a sense of unease.
When an individual regains consciousness after a vasovagal syncope episode, they may feel a surge of anxiety and fear due to the disorienting experience they just went through. Confusion may set in as they try to piece together what happened during the period of unconsciousness. The sudden loss of control over their own body can leave them feeling uneasy and vulnerable. These emotional and psychological responses are primarily a result of the abrupt loss of consciousness and the overall experience of a vasovagal syncope episode.
Diagnostic Procedures for Vasovagal Syncope with Convulsions
When a person experiences vasovagal syncope with convulsions, it is crucial to undergo proper diagnostic procedures to determine the underlying cause and rule out other potential conditions. The diagnostic process typically involves a thorough medical history review, physical examination, and specialized tests and procedures:
Medical History and Physical Examination
The medical history review and physical examination are essential in identifying any potential underlying factors that contribute to vasovagal syncope. During the medical history review, the healthcare provider may inquire about the frequency and duration of episodes, potential triggers, and any relevant medical conditions. This comprehensive evaluation allows the healthcare provider to gather crucial information that may help in the diagnosis and management of vasovagal syncope.
Furthermore, the physical examination aims to assess the person’s overall health, including heart function, blood pressure, and neurological examination. The healthcare provider will carefully listen to the patient’s heart sounds, check for any abnormalities, and evaluate the person’s blood pressure to identify any potential issues that may contribute to vasovagal syncope. Additionally, a neurological examination may be conducted to assess the person’s nervous system and identify any abnormalities that may be associated with the condition.
Specialized Tests and Procedures
In some cases, specialized tests and procedures may be necessary to confirm the diagnosis of vasovagal syncope and investigate any underlying causes or contributing factors. These tests provide valuable insights into the person’s cardiovascular system and help determine the appropriate treatment approach.
One of the commonly used tests is an electrocardiogram (ECG), which evaluates the electrical activity of the heart. This non-invasive test allows healthcare providers to assess the heart’s rhythm and detect any abnormalities that may contribute to vasovagal syncope. By analyzing the ECG results, healthcare providers can gain valuable information about the person’s heart function and identify any potential cardiac issues.
In addition to an ECG, a tilt-table test may be recommended to provoke and observe syncope episodes. During this test, the person lies on a table that can be tilted to different angles. The healthcare provider closely monitors the person’s blood pressure, heart rate, and symptoms while changing the table’s position. This test helps replicate the conditions that may trigger vasovagal syncope and allows healthcare providers to observe the person’s response, aiding in the diagnosis and understanding of the condition.
Furthermore, echocardiography, a non-invasive imaging test, may be performed to assess the structure and function of the heart. This test uses sound waves to create detailed images of the heart, providing valuable information about its size, shape, and how well it is pumping blood. By evaluating the heart’s structure and function, healthcare providers can identify any abnormalities that may contribute to vasovagal syncope and guide the appropriate treatment plan.
It is important to note that the diagnostic procedures mentioned above are not exhaustive, and healthcare providers may recommend additional tests or procedures based on the individual’s specific case. The goal is to gather as much information as possible to accurately diagnose vasovagal syncope and determine the most effective treatment approach. Through a comprehensive diagnostic process, healthcare providers can provide appropriate care and help individuals manage their condition effectively.
Treatment Options for Vasovagal Syncope with Convulsions
While there is no specific cure for vasovagal syncope, several treatment options can help manage the condition and reduce the frequency and severity of episodes. The treatment approach may vary depending on the underlying causes, triggers, and individual factors:
Medication and Drug Therapies
In some cases, medication may be prescribed to manage vasovagal syncope and prevent fainting episodes. These medications aim to regulate heart rate and blood pressure to minimize the chances of sudden drops. It is crucial to discuss the potential risks and benefits of medication therapy with a healthcare professional, as they can have side effects and interact with other medications.
One commonly prescribed medication for vasovagal syncope is beta-blockers. These medications work by blocking the effects of adrenaline on the heart, helping to reduce heart rate and blood pressure. Beta-blockers can be effective in preventing fainting episodes, but they may also cause side effects such as fatigue, dizziness, and low blood pressure.
In addition to beta-blockers, other medications such as fludrocortisone may be prescribed. Fludrocortisone is a synthetic steroid that helps increase blood volume and blood pressure, reducing the likelihood of fainting. However, it is important to monitor blood pressure regularly while taking this medication, as it can cause fluid retention and electrolyte imbalances.
Lifestyle Changes and Home Remedies
Implementing certain lifestyle changes and home remedies can help manage vasovagal syncope effectively. These may include maintaining a well-balanced diet, staying hydrated, avoiding triggers such as prolonged standing or extreme temperatures, and learning stress management techniques. It is important to note that lifestyle changes alone may not eliminate the occurrence of vasovagal syncope, but they can significantly reduce the frequency and severity of episodes.
A well-balanced diet is essential for overall cardiovascular health. Including foods rich in potassium, such as bananas, oranges, and spinach, can help regulate blood pressure. Additionally, consuming foods high in magnesium, such as nuts, seeds, and dark chocolate, can help relax blood vessels and improve blood flow.
Staying hydrated is also crucial in managing vasovagal syncope. Dehydration can lead to low blood volume, which can trigger fainting episodes. Drinking an adequate amount of water throughout the day, especially in hot weather or during physical activity, can help maintain proper hydration levels.
Triggers such as prolonged standing or extreme temperatures can provoke vasovagal syncope episodes. It is important to identify and avoid these triggers whenever possible. Taking breaks, sitting or lying down when feeling lightheaded, and avoiding hot baths or saunas can help prevent fainting episodes.
Learning stress management techniques can also be beneficial in managing vasovagal syncope. Stress and anxiety can trigger the body’s “fight or flight” response, leading to changes in heart rate and blood pressure. Engaging in activities such as deep breathing exercises, meditation, yoga, or engaging in hobbies can help reduce stress levels and promote relaxation.
Surgical and Other Medical Interventions
In severe cases or when other treatment options do not provide sufficient relief, surgical and other medical interventions may be considered. These interventions aim to address underlying heart conditions or nerve abnormalities that contribute to vasovagal syncope. It is essential to consult with a healthcare professional to assess the potential risks, benefits, and appropriateness of such interventions.
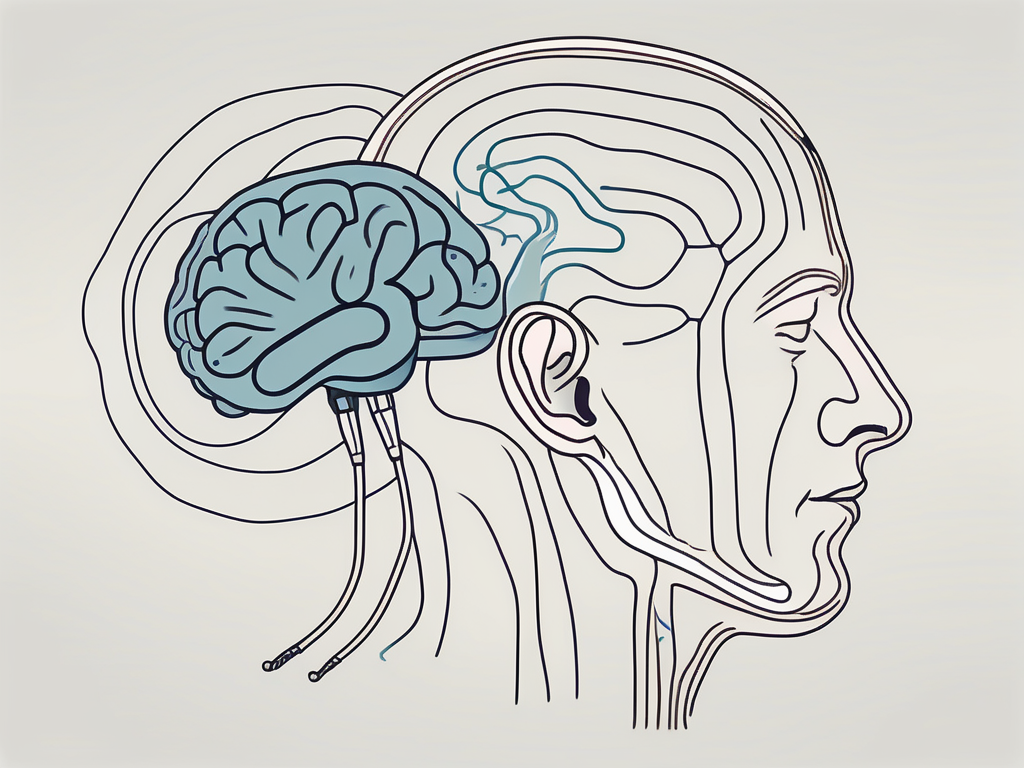
One surgical intervention that may be considered is the implantation of a pacemaker. A pacemaker is a small device that is surgically placed under the skin near the collarbone. It helps regulate the heart’s electrical signals and can prevent sudden drops in heart rate, reducing the likelihood of fainting episodes.
In some cases, a procedure called cardiac ablation may be recommended. Cardiac ablation involves using heat or cold energy to destroy small areas of heart tissue that may be causing abnormal electrical signals. This procedure can help restore normal heart rhythm and reduce the occurrence of vasovagal syncope episodes.
Other medical interventions, such as nerve stimulation or tilt table testing, may also be considered depending on the individual’s specific condition and symptoms. These interventions aim to identify and address the underlying causes of vasovagal syncope, providing relief and improving quality of life.
Living with Vasovagal Syncope and Convulsions
Living with vasovagal syncope and convulsions can be challenging, but there are coping mechanisms and strategies that can help individuals manage the condition and improve their quality of life:
Coping Mechanisms and Strategies
Developing effective coping mechanisms and strategies can assist individuals in dealing with vasovagal syncope episodes when they occur. This can include learning relaxation techniques, deep breathing exercises, and recognizing early warning signs of an episode. Understanding and accepting the condition can also play a significant role in coping with the emotional and psychological aspects associated with vasovagal syncope.
Support Systems and Resources
Building a strong support system and accessing relevant resources can make living with vasovagal syncope easier. Support groups, online communities, and educational materials can be valuable sources of information, empathy, and encouragement. Moreover, it is essential to communicate openly with healthcare professionals, family members, and friends to ensure understanding and appropriate support.
Prevention and Risk Reduction of Vasovagal Syncope with Convulsions
Prevention and risk reduction are key aspects of managing vasovagal syncope and minimizing the likelihood of fainting episodes. While it may not be possible to completely prevent vasovagal syncope, certain measures can be taken to reduce the risk:
Healthy Habits and Routine Check-ups
Maintaining a healthy lifestyle, which includes regular exercise, balanced nutrition, and adequate hydration, can contribute to overall well-being and potentially reduce the frequency of vasovagal syncope episodes. Additionally, routine check-ups with a healthcare professional allow for regular monitoring of heart health and the identification of any changes or underlying conditions that may contribute to syncope episodes.
Understanding and Avoiding Triggers
Identifying and understanding individual triggers can greatly help in preventing vasovagal syncope episodes. This includes knowing the situations, activities, or substances that tend to provoke a response, such as excessive stress, heat exposure, or specific medications. By avoiding these triggers or implementing necessary precautions, the risk of vasovagal syncope and convulsions can be significantly reduced.
In conclusion, vasovagal syncope with convulsions is a complex condition that can significantly impact an individual’s quality of life. Understanding its causes, recognizing symptoms, seeking appropriate medical evaluation, and implementing appropriate management strategies are key to mitigating the effects of vasovagal syncope. If you or someone you know experiences fainting episodes with convulsions, it is crucial to consult with a healthcare professional for proper diagnosis, treatment, and guidance.




Leave a Reply