Vasovagal syncope and diarrhea are two medical conditions that often occur in conjunction with each other. While they may seem unrelated at first, there is a clear connection between the two. In this article, we will delve into the intricacies of vasovagal syncope, diarrhea, and the link that ties them together. It is important to note that the information provided here is for informational purposes only and should not be considered as medical advice. If you are experiencing any symptoms or have concerns about your health, please consult with a healthcare professional.
Defining Vasovagal Syncope
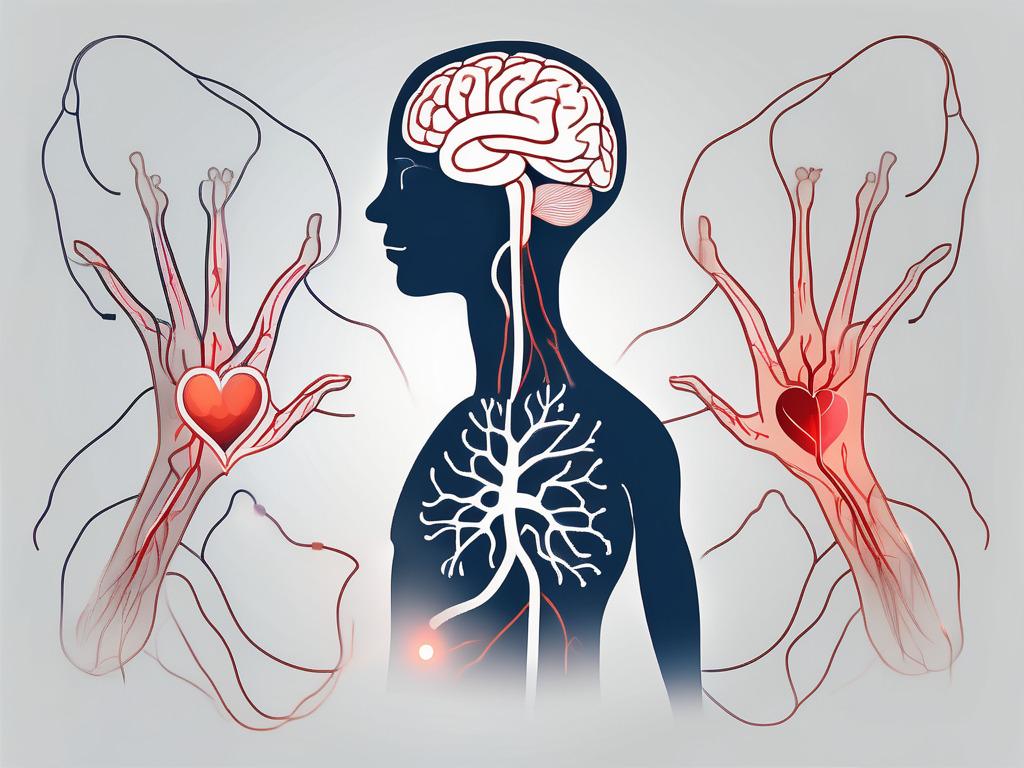
Vasovagal syncope, also known as neurocardiogenic syncope or reflex syncope, is a common cause of fainting episodes. It occurs when there is a sudden drop in blood pressure, leading to a temporary reduction in blood flow to the brain. This, in turn, causes a person to lose consciousness momentarily.
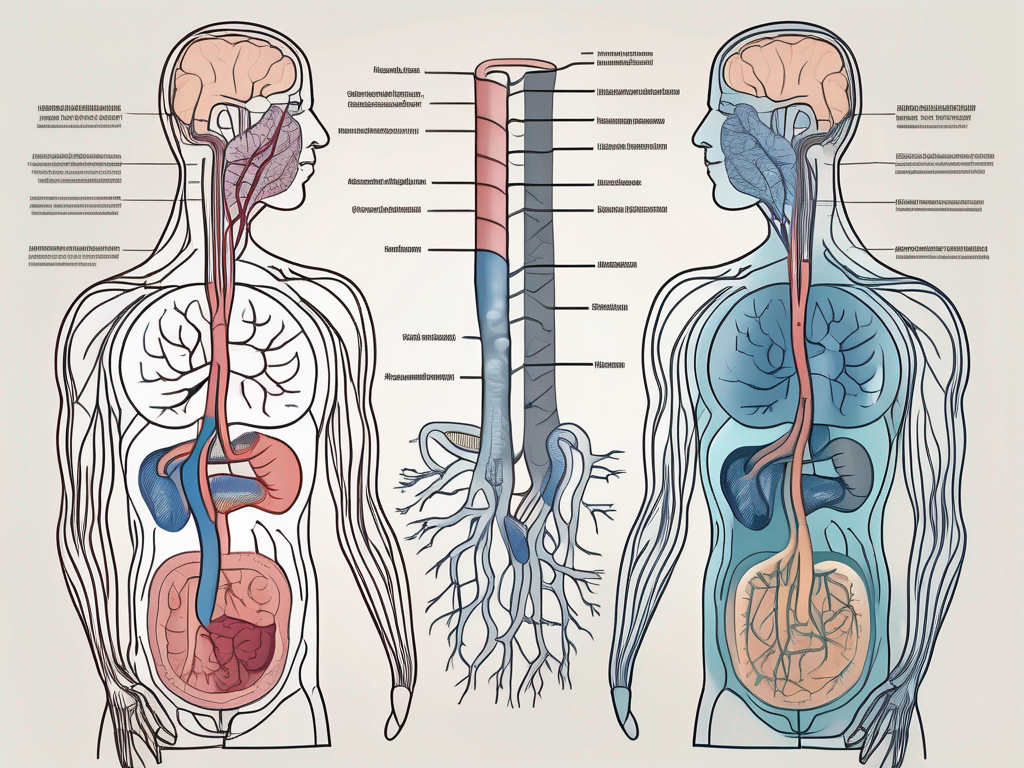
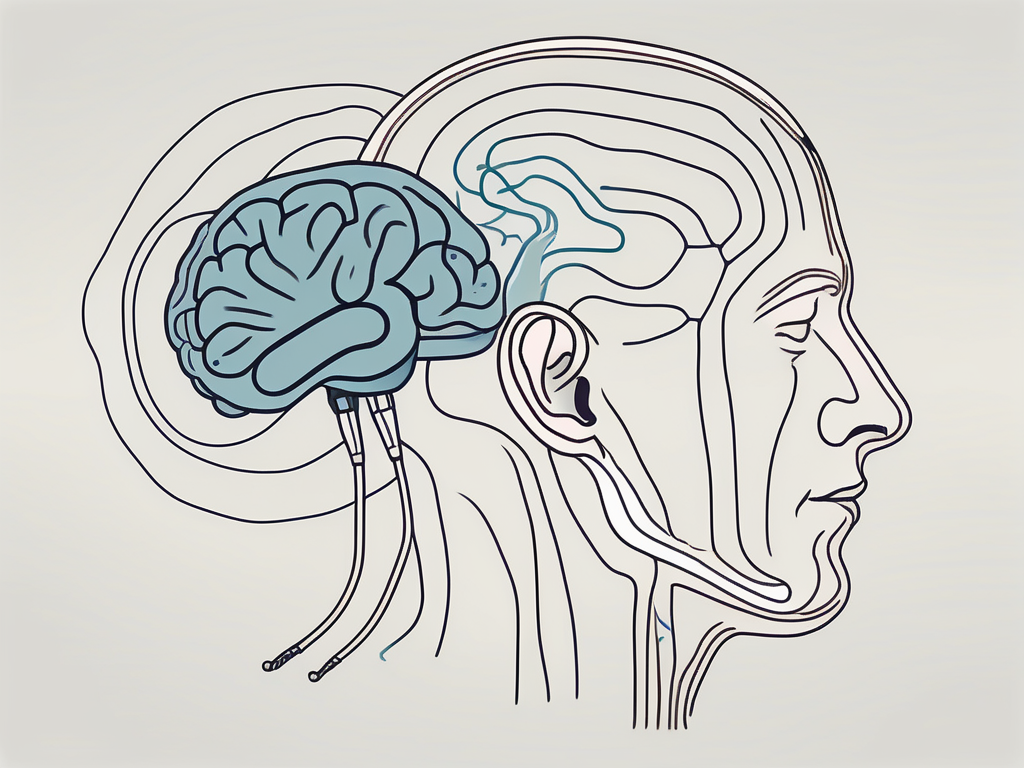
While the exact mechanisms behind vasovagal syncope are not yet fully understood, it is believed to be triggered by the activation of the vagus nerve. The vagus nerve is a vital component of the parasympathetic nervous system, responsible for regulating various bodily functions, including heart rate, blood pressure, and digestion.
The Role of the Vagus Nerve in Vasovagal Syncope
The vagus nerve plays a crucial role in vasovagal syncope. When the body detects certain triggers, such as stress, fear, pain, or even standing up too quickly, the vagus nerve becomes stimulated and sends signals to slow down the heart rate and dilate blood vessels. This response is intended to redirect blood flow to vital organs, including the brain, as a defense mechanism against potentially harmful situations.
However, in some individuals, the vagus nerve may become hyperactive or overly sensitive, leading to an exaggerated response. This can result in a sudden drop in blood pressure and heart rate, causing fainting episodes characteristic of vasovagal syncope.
In addition to its role in vasovagal syncope, the vagus nerve is also involved in other physiological processes. It plays a crucial role in digestion, controlling the movement of food through the digestive tract and promoting the release of digestive enzymes. The vagus nerve also helps regulate breathing, influencing the rate and depth of breaths taken. Furthermore, it is involved in the body’s stress response, helping to dampen the effects of the sympathetic nervous system and promote relaxation.
Common Triggers of Vasovagal Syncope
Vasovagal syncope can be triggered by a variety of factors, including emotional stress, intense fear or pain, prolonged standing, heat exposure, dehydration, and blood loss. Some individuals may also experience syncope episodes during certain activities, such as swallowing, coughing, or having a bowel movement.
It is important to note that while these triggers may be common among individuals with vasovagal syncope, each person’s triggers can vary. Some individuals may find that certain smells, sounds, or even specific foods can trigger a fainting episode. Understanding and identifying personal triggers is crucial in managing and preventing syncope episodes.
Managing vasovagal syncope often involves a combination of lifestyle modifications and medical interventions. Lifestyle modifications may include avoiding known triggers, staying hydrated, maintaining a healthy diet, and practicing stress-reducing techniques such as deep breathing or meditation. In some cases, medications may be prescribed to help regulate heart rate and blood pressure or to reduce the sensitivity of the vagus nerve.
While vasovagal syncope can be a challenging condition to live with, understanding its underlying mechanisms and triggers can empower individuals to take control of their health and minimize the impact of fainting episodes on their daily lives.
Understanding Diarrhea
Diarrhea is a condition characterized by loose, watery stools that occur more frequently than usual. It is often accompanied by abdominal pain, cramping, bloating, and an urgent need to use the restroom. While diarrhea can be a temporary inconvenience, it can also be a symptom of an underlying health issue.
When it comes to understanding diarrhea, it’s important to explore the various causes that can contribute to this condition. There are numerous potential causes of diarrhea, including infections, food intolerances, medications, and underlying medical conditions.
Causes of Diarrhea
Infectious causes of diarrhea often include viral, bacterial, or parasitic infections that affect the digestive system. These infections can be acquired through contaminated food or water, poor hygiene practices, or close contact with an infected individual.
Food intolerances, such as lactose intolerance or gluten sensitivity, can also lead to diarrhea in some individuals. When the body is unable to properly digest certain substances, it can result in gastrointestinal symptoms, including diarrhea.
Additionally, certain medications, such as antibiotics or laxatives, can disrupt the balance of bacteria in the gut and result in diarrhea as a side effect. Antibiotics, while effective in treating bacterial infections, can also unintentionally kill off beneficial bacteria in the gut, leading to digestive disturbances.
In some cases, diarrhea may be a symptom of an underlying medical condition, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or celiac disease. These conditions require proper diagnosis and management by a healthcare professional. It is important to seek medical attention if diarrhea persists or is accompanied by other concerning symptoms.
The Impact of Diarrhea on the Body
Diarrhea can have a significant impact on the body’s overall well-being, especially if it persists or becomes chronic. One of the primary concerns with diarrhea is dehydration. When the body loses excessive amounts of water through loose stools, it can lead to dehydration, which can be particularly dangerous for young children, older adults, and individuals with weakened immune systems.
In addition to dehydration, diarrhea can also cause electrolyte imbalances. Electrolytes, such as sodium, potassium, and chloride, play a crucial role in maintaining proper fluid balance and nerve function in the body. When diarrhea occurs, these electrolytes can be lost in excessive amounts, leading to imbalances that can further exacerbate symptoms.
Furthermore, chronic diarrhea can result in nutrient deficiencies and malnutrition. The body relies on the absorption of nutrients from food to function properly. When diarrhea is persistent, the body may not have enough time to absorb essential nutrients, leading to deficiencies that can impact overall health and well-being.
In severe cases, diarrhea can also cause weight loss and weaken the immune system. The constant loss of fluids and nutrients can lead to unintentional weight loss, which can be concerning. Additionally, the immune system can become compromised, leaving individuals more susceptible to infections and illnesses.
It is important to address diarrhea promptly and seek medical attention if it persists or is accompanied by severe symptoms. Proper diagnosis and management can help alleviate symptoms, treat the underlying cause, and prevent potential complications.
The Connection Between Vasovagal Syncope and Diarrhea
Although vasovagal syncope and diarrhea may seem unrelated on the surface, there is a significant connection between the two conditions. The autonomic nervous system, which includes the vagus nerve, plays a crucial role in regulating various bodily functions, including both the cardiovascular and digestive systems.
The Role of the Autonomic Nervous System
The autonomic nervous system is responsible for maintaining the body’s homeostasis by controlling involuntary actions, such as heart rate, blood pressure, digestion, and bowel movements. It consists of two divisions: the sympathetic nervous system, which activates the “fight or flight” response, and the parasympathetic nervous system, which promotes a state of relaxation and optimal organ function.
In certain individuals, the autonomic nervous system may become dysregulated, leading to an imbalance between the sympathetic and parasympathetic divisions. This dysregulation can manifest as both vasovagal syncope and gastrointestinal symptoms, including diarrhea.
How Diarrhea Can Trigger Vasovagal Syncope
In some cases, the act of having a bowel movement, specifically straining during defecation, can increase intra-abdominal pressure. This increased pressure can activate the vagus nerve, leading to a vasovagal response that causes a drop in blood pressure and fainting episodes. This phenomenon is known as defecation syncope.
While defecation syncope is relatively rare, it highlights the intricate connection between the gastrointestinal system and the cardiovascular system. Individuals with a history of vasovagal syncope may be more susceptible to these episodes triggered by bowel movements.
It is important to note that the relationship between vasovagal syncope and diarrhea is not limited to defecation syncope. Other factors, such as certain medications, dietary triggers, and underlying medical conditions, can also contribute to the occurrence of both vasovagal syncope and diarrhea.
For instance, some medications used to treat cardiovascular conditions, such as beta blockers, can affect the autonomic nervous system and potentially lead to gastrointestinal symptoms, including diarrhea. Additionally, certain foods or food intolerances can trigger both vasovagal syncope and diarrhea in susceptible individuals.
Furthermore, individuals with conditions such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD) may experience episodes of vasovagal syncope in conjunction with diarrhea. These conditions are characterized by chronic inflammation in the gastrointestinal tract, which can disrupt the normal functioning of the autonomic nervous system and lead to dysregulation.
In conclusion, while vasovagal syncope and diarrhea may appear unrelated, they share a complex relationship mediated by the autonomic nervous system. Dysregulation of this system can result in both cardiovascular and gastrointestinal symptoms, including fainting episodes and diarrhea. Understanding this connection is crucial for healthcare professionals to provide comprehensive care to individuals experiencing these conditions.
Symptoms and Diagnosis of Vasovagal Syncope and Diarrhea
Recognizing the symptoms of vasovagal syncope and diarrhea is vital for proper diagnosis and management. Both conditions have distinct signs and symptoms that can help differentiate them from other medical issues.
Recognizing the Symptoms
The primary symptom of vasovagal syncope is a sudden loss of consciousness that is often preceded by lightheadedness, dizziness, or nausea. Fainting episodes are typically brief and are followed by a rapid recovery once adequate blood flow to the brain is restored.
It is important to note that vasovagal syncope can be triggered by various factors, such as emotional stress, pain, dehydration, or even prolonged standing. These triggers can activate the vagus nerve, leading to a sudden drop in heart rate and blood pressure, resulting in syncope.
In contrast, the symptoms of diarrhea include frequent loose stools, abdominal pain, cramping, bloating, and a sense of urgency to have a bowel movement. The severity and duration of symptoms may vary depending on the underlying cause.
Diarrhea can be caused by a multitude of factors, including viral or bacterial infections, food intolerances, medication side effects, or underlying gastrointestinal conditions. Identifying the specific cause is crucial for effective treatment and management.
Diagnostic Tests and Procedures
Diagnosing vasovagal syncope and diarrhea involves a thorough evaluation of medical history, physical examination, and, when necessary, additional tests or consultations with specialists.
In the case of vasovagal syncope, doctors may employ a variety of diagnostic tools, including electrocardiograms (ECGs) to assess heart function, tilt-table testing to provoke syncope episodes under controlled conditions, and blood tests to rule out other potential causes of fainting episodes.
Furthermore, a detailed assessment of the patient’s medical history is crucial in identifying any triggers or underlying conditions that may contribute to vasovagal syncope. This may involve discussions about the patient’s lifestyle, occupation, stress levels, and any previous episodes of syncope.
To diagnose diarrhea, doctors may conduct stool tests to detect any infectious pathogens, blood tests to assess for inflammation or malabsorption, and imaging studies, such as colonoscopies or imaging scans, to evaluate the health of the gastrointestinal tract.
In some cases, doctors may recommend a dietary evaluation to identify any potential food intolerances or allergies that could be contributing to the diarrhea. Additionally, a thorough review of the patient’s medication history is essential to determine if any medications may be causing or exacerbating the symptoms.
Overall, the diagnosis of vasovagal syncope and diarrhea requires a comprehensive approach that takes into account the patient’s symptoms, medical history, and the results of various diagnostic tests. This allows healthcare professionals to develop an individualized treatment plan that addresses the underlying causes and provides effective symptom management.
Treatment Options for Vasovagal Syncope and Diarrhea
Treatment for vasovagal syncope and diarrhea focuses on managing symptoms, identifying triggers, and preventing recurrent episodes. It is essential for individuals to work closely with their healthcare providers to develop a personalized treatment plan.
Lifestyle Changes and Home Remedies
In some cases, lifestyle modifications and home remedies may effectively reduce the frequency and severity of vasovagal syncope and diarrhea episodes. These may include:
- Avoiding known triggers, such as prolonged standing or emotional stress
- Maintaining adequate hydration
- Practicing relaxation techniques, such as deep breathing or meditation
- Following a balanced diet and avoiding foods that trigger diarrhea
It is important to note that while these measures may provide relief for some individuals, they may not be sufficient in all cases. Consulting with a healthcare professional is essential to determine the most appropriate course of treatment.
Medications and Therapies
In certain cases, medication or specialized therapies may be prescribed to manage vasovagal syncope and diarrhea.
For vasovagal syncope, doctors may prescribe medications, such as beta-blockers or fludrocortisone, to help regulate heart rate and blood pressure. Additionally, in some situations, cardiac pacing devices may be implanted to prevent bradycardia or chronotropic incompetence.
The treatment for diarrhea depends on the underlying cause. Antidiarrheal medications, such as loperamide, may be prescribed to alleviate symptoms temporarily. However, addressing the root cause of the diarrhea is essential for long-term management. This may involve supportive measures, dietary modifications, or specific treatments targeted at the underlying condition.
Prevention Strategies for Vasovagal Syncope and Diarrhea
While it may not always be possible to prevent every episode of vasovagal syncope or diarrhea, certain strategies can help minimize the occurrence and impact of these conditions.
Dietary Recommendations
For individuals prone to vasovagal syncope and diarrhea, making appropriate dietary choices can make a difference. Ensuring an optimal intake of fluids and electrolytes can help maintain hydration and support normal bodily functions.
People experiencing diarrhea should consider incorporating foods that are easier to digest and less likely to trigger symptoms. This may include bland foods, such as bananas, rice, applesauce, and toast (BRAT diet), as well as low-fiber options.
Exercise and Stress Management Techniques
Regular physical activity and stress management techniques can contribute to the overall well-being of individuals prone to vasovagal syncope and diarrhea.
Engaging in gentle exercise, such as walking or yoga, can help promote cardiovascular health and reduce stress levels. Additionally, practicing relaxation techniques, such as deep breathing exercises or mindfulness meditation, can aid in stress management and potentially reduce the frequency and severity of syncope episodes.
The Long-Term Outlook for Individuals with Vasovagal Syncope and Diarrhea
While vasovagal syncope and diarrhea can significantly impact an individual’s quality of life, with proper management and lifestyle adjustments, most people can lead relatively normal lives.
Potential Complications
Vasovagal syncope can occasionally lead to injuries or accidents if fainting episodes occur at inappropriate times or in hazardous environments. Therefore, it is crucial for individuals with vasovagal syncope to be aware of their triggers and take necessary precautions to ensure their safety.
Prolonged or recurrent diarrhea can lead to complications such as dehydration, electrolyte imbalances, and malnutrition. If left untreated, these complications can have a significant impact on an individual’s overall health and well-being.
Living with Vasovagal Syncope and Diarrhea
Living with vasovagal syncope and diarrhea can be challenging, but it is important to remember that there are various management strategies and support available. Connecting with healthcare professionals, support groups, or online communities can provide valuable guidance and reassurance.
In conclusion, understanding the link between vasovagal syncope and diarrhea requires a comprehensive knowledge of the cardiovascular and digestive systems. While the connection may not be immediately apparent, it is through a deeper understanding of these conditions that healthcare professionals can diagnose and manage their patients effectively. It is crucial for individuals experiencing symptoms to consult with qualified medical professionals to obtain accurate diagnoses and appropriate treatment plans tailored to their specific needs.




Leave a Reply