The vasovagal response to needles is a complex and fascinating phenomenon that can cause discomfort and even fainting in some individuals. It is important to understand this response, its causes, symptoms, and management strategies to ensure the wellbeing of those who may experience it. In this article, we will delve into the physiology behind the vasovagal response, examine the connection between needles and this response, identify the symptoms, explore the causes, discuss management techniques, and touch upon medical treatments and lifestyle adjustments that can help individuals living with vasovagal syncope.
What is the Vasovagal Response?
Before delving into the intricacies of the vasovagal response, let’s first understand what it actually entails. The vasovagal response is a reflex action that occurs when the body overreacts to certain triggers, resulting in a sudden decrease in heart rate and blood pressure. This can lead to a feeling of lightheadedness, dizziness, and in extreme cases, fainting. The vasovagal response is believed to be a protective mechanism evolved over time.
The Physiology Behind Vasovagal Syncope
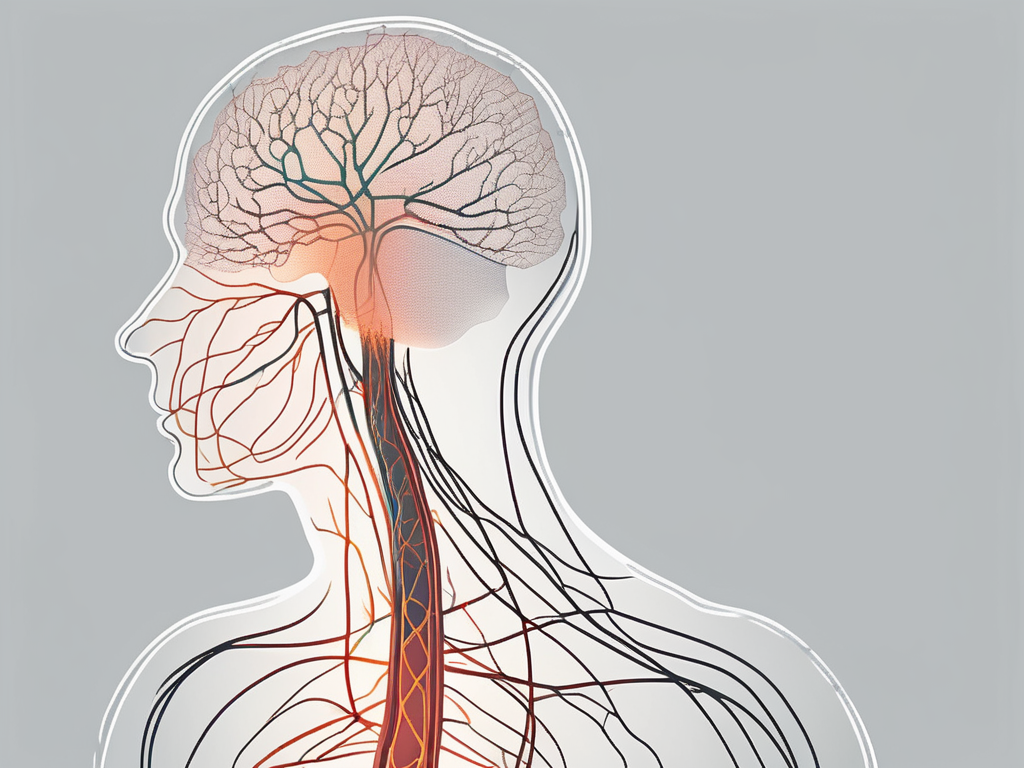
To understand why the vasovagal response occurs, we must explore its underlying physiology. During a vasovagal episode, the vagus nerve, which plays a significant role in regulating heart rate and blood pressure, becomes overly active. This nerve stimulates the release of acetylcholine, a neurotransmitter that slows down the heart and relaxes blood vessels, causing blood pressure to drop abruptly.
Additionally, the body releases stress hormones, such as adrenaline and cortisol, in response to the perceived threat or trigger. This hormonal reaction can amplify the physical symptoms experienced during a vasovagal response.
Furthermore, the vasovagal response involves a complex interplay between the autonomic nervous system, which controls involuntary bodily functions, and the cardiovascular system. The autonomic nervous system consists of two branches: the sympathetic nervous system, responsible for the “fight or flight” response, and the parasympathetic nervous system, responsible for the “rest and digest” response. In the case of the vasovagal response, the parasympathetic nervous system becomes dominant, leading to the characteristic drop in heart rate and blood pressure.
Triggers of Vasovagal Response
The vasovagal response can be triggered by various factors. Common triggers include the sight of blood, severe pain, emotional distress, standing for prolonged periods, and, of course, the anticipation or experience of needles. It is important to note that triggers can vary from person to person, and what may cause a vasovagal response in one individual may not affect another.
When it comes to the sight of blood, the vasovagal response can be particularly strong. This is thought to be an evolutionary adaptation, as a sudden drop in heart rate and blood pressure may have helped our ancestors conserve blood and minimize bleeding in case of injury.
Severe pain can also trigger a vasovagal response. This is believed to be a protective mechanism, as the body’s response to pain involves releasing endorphins, which can cause a drop in blood pressure.
Emotional distress, such as fear or anxiety, can also elicit a vasovagal response. The body’s stress response, triggered by emotional stimuli, can activate the vagus nerve and lead to a decrease in heart rate and blood pressure.
Standing for prolonged periods, especially in hot environments, can cause blood to pool in the legs and lower body. This pooling of blood can activate the vasovagal response as a way to redirect blood flow and prevent fainting.
Lastly, the anticipation or experience of needles is a common trigger for the vasovagal response. This is believed to be a combination of the body’s natural aversion to pain and the psychological factors associated with medical procedures.
Overall, the vasovagal response is a fascinating physiological phenomenon that involves intricate interactions between the nervous system, cardiovascular system, and emotional factors. Understanding its triggers and underlying mechanisms can help individuals recognize and manage this reflex action effectively.
The Connection Between Needles and Vasovagal Response
When it comes to needles, both the psychological aspect and the physical reaction contribute to the vasovagal response.
Needles, although small in size, have the power to evoke strong emotions in many individuals. The mere thought of a needle can trigger anxiety and fear, causing a cascade of physiological responses. This psychological aspect plays a significant role in the development of a vasovagal response.
For some, the fear of needles stems from past traumatic experiences, such as painful injections or medical procedures. These memories can become deeply ingrained in the subconscious mind, creating a conditioned response of fear and anxiety. As a result, the anticipation of a needle can activate the body’s fight or flight response, leading to an elevated heart rate and increased blood pressure.
Furthermore, the fear of needles is not limited to those with a history of trauma. It is a common phobia that affects a significant portion of the population. The fear may be rooted in the fear of pain, the fear of blood, or even the fear of the unknown. Regardless of the specific cause, the psychological response to needles can be intense and overwhelming.
The Psychological Aspect
For many people, the mere thought of needles can trigger anxiety and fear. This psychological response can activate the body’s fight or flight response, resulting in an elevated heart rate and increased blood pressure. These reactions, combined with the already sensitive vagus nerve, can pave the way for a vasovagal episode.
It is important to note that the psychological aspect of the vasovagal response is not solely limited to fear and anxiety. Some individuals may experience a vasovagal response due to other psychological factors, such as disgust or even anticipation. The mind plays a powerful role in shaping our physical reactions, and the vasovagal response is no exception.
Moreover, the psychological aspect of the vasovagal response can vary from person to person. While some individuals may be able to overcome their fear of needles through therapy or desensitization techniques, others may find it challenging to manage their anxiety. Understanding the psychological aspect of the vasovagal response is crucial in developing effective strategies for prevention and management.
The Physical Reaction
When a needle is inserted into the body, it can stimulate the vagus nerve directly or indirectly, triggering the vasovagal response. Studies have shown that the physical act of needle penetration can cause a reflexive reaction, regardless of the individual’s emotional state. This physical reaction, coupled with the psychological stress, can create a perfect storm leading to a vasovagal response.
The vagus nerve, also known as the “wandering nerve,” is responsible for regulating various bodily functions, including heart rate, blood pressure, and digestion. It is highly sensitive and can be easily stimulated by external factors, such as the insertion of a needle. When the vagus nerve is activated, it sends signals to the brain, resulting in a decrease in heart rate and blood pressure.
Interestingly, the physical reaction to needle insertion can vary among individuals. Some may experience a vasovagal response immediately upon needle penetration, while others may have a delayed response. The exact mechanisms behind these variations are still not fully understood and require further research.
It is worth noting that the physical reaction to needles is not limited to the vasovagal response. Some individuals may experience other physiological responses, such as dizziness, nausea, or even fainting. These reactions can further complicate medical procedures and require careful management by healthcare professionals.
In conclusion, the connection between needles and the vasovagal response is multifaceted, involving both psychological and physical factors. The fear and anxiety associated with needles can activate the body’s fight or flight response, while the physical act of needle penetration can directly stimulate the vagus nerve. Understanding these connections is crucial in providing appropriate care and support for individuals who experience vasovagal episodes in response to needles.
Identifying the Symptoms of a Vasovagal Response to Needles
Recognizing the symptoms of a vasovagal response is crucial, as it allows individuals and healthcare professionals to manage and respond appropriately. Symptoms can be categorized into immediate and delayed symptoms.
A vasovagal response, also known as a vasovagal syncope, is a common reaction that occurs in some individuals when they are exposed to certain triggers, such as needles. It is a reflex response that involves the involuntary nervous system, resulting in a temporary decrease in blood flow to the brain. Understanding the symptoms associated with this response can help individuals and healthcare professionals provide appropriate care and support.
Immediate Symptoms
During a vasovagal response, individuals may experience a sudden feeling of warmth, sweating, paleness, lightheadedness, or dizziness. These symptoms can be alarming and may cause individuals to feel anxious or frightened. It is important to note that these symptoms are typically short-lived and resolve on their own once the trigger has been removed.
In some cases, the vasovagal response can be more severe, leading to a loss of consciousness. This can be a distressing experience for both the individual and those around them. It is important to ensure that the person is in a safe position to prevent any injuries that may occur during a fainting episode.
In addition to the physical symptoms, individuals may also experience emotional distress during a vasovagal response. The sudden onset of symptoms can be overwhelming and may cause individuals to feel scared or anxious. It is important to provide reassurance and support to help them through this challenging experience.
Delayed Symptoms
After the immediate symptoms subside, individuals may experience lingering effects such as fatigue, muscle aches, headaches, and difficulty concentrating. These delayed symptoms are temporary and usually resolve on their own within a short period.
It is important to note that while vasovagal responses can be uncomfortable and distressing, they are generally harmless and do not pose any long-term health risks. However, if you or someone you know experiences frequent or severe vasovagal responses, it is advisable to consult a healthcare professional for further evaluation and guidance.
Managing a vasovagal response involves identifying and avoiding triggers whenever possible. For individuals who require medical procedures involving needles, healthcare professionals can employ various techniques to help minimize the likelihood of a vasovagal response. These may include distracting the individual, using numbing creams or sprays, or adjusting the positioning during the procedure.
Overall, understanding the symptoms of a vasovagal response can help individuals and healthcare professionals effectively manage and respond to this common reaction. By providing appropriate care and support, individuals can navigate through the experience with greater ease and confidence.
Causes of Vasovagal Response to Needles
Understanding the causes of the vasovagal response to needles requires examining both inherent and environmental factors. The vasovagal response, also known as a vasovagal episode or vasovagal syncope, is a common physiological reaction that can occur during needle procedures.
When a person experiences a vasovagal response, their body overreacts to certain triggers, causing a sudden drop in heart rate and blood pressure. This can result in dizziness, lightheadedness, and, in extreme cases, fainting. It is important to explore the various factors that can contribute to this response to better understand and manage it.
Inherent Factors
Some individuals may have a genetic predisposition to the vasovagal response, making them more susceptible to needle-related triggers. Research suggests that certain genetic variations can influence the body’s autonomic nervous system, which regulates heart rate and blood pressure. These genetic factors can make some individuals more prone to experiencing a vasovagal response during needle procedures.
It is beneficial for individuals to be aware of their family medical history and discuss it with their healthcare provider to establish if such a predisposition exists. By understanding their inherent factors, individuals can take proactive measures to manage their vasovagal response and minimize its impact on their overall well-being.
Environmental Factors
Environmental factors, such as the setting in which the needle procedure takes place, can also play a significant role in triggering a vasovagal response. The physical environment can have a profound impact on an individual’s emotional and physiological state, potentially exacerbating their response to needles.
Factors like temperature, lighting, stress, and the presence of medical equipment can all influence an individual’s response. For example, a cold and sterile environment may heighten anxiety and discomfort, increasing the likelihood of a vasovagal episode. On the other hand, a warm and soothing environment can promote relaxation and help alleviate the stress associated with needle procedures.
Healthcare professionals can play a crucial role in creating a calm and comfortable environment for their patients. By being mindful of these environmental factors and making necessary adjustments, healthcare providers can help minimize the chances of a vasovagal episode and enhance the overall experience for their patients.
In conclusion, the causes of the vasovagal response to needles are multifaceted, involving both inherent and environmental factors. By understanding and addressing these factors, individuals and healthcare providers can work together to manage and mitigate the impact of vasovagal episodes during needle procedures.
Managing a Vasovagal Response to Needles
Managing a vasovagal response involves a combination of precautionary measures, actions during an episode, and post-episode care.
Precautionary Measures
Before any needle-related procedure, healthcare providers should assess the patient’s medical history, including a detailed discussion of any previous vasovagal responses. This evaluation can help determine the necessity of certain procedures and guide management strategies accordingly. Additionally, informing healthcare professionals about the fear or anxiety of needles can provide them with valuable insights to adapt their approach during the procedure.
Patients are advised to communicate openly with their healthcare providers about any concerns or fears they may have. Establishing a sense of trust and ensuring the patient feels heard can go a long way in managing their vasovagal response effectively.
During the Episode
If an individual experiences a vasovagal response during a needle-related procedure, healthcare professionals should promptly respond by ensuring the patient’s safety. This may involve stopping the procedure, reclining the patient to promote blood flow to the brain, and providing emotional support. However, it is important to note that the specific actions taken should be based on the individual’s condition and the healthcare professional’s expertise.
It is essential to reiterate that individuals should consult with their healthcare providers for personalized advice and management strategies.
Post-Episode Care
After experiencing a vasovagal response, it is advisable for individuals to take some time to rest and recover. Deep breathing exercises and maintaining hydration can help stabilize blood pressure and reduce symptoms. If symptoms persist or worsen after an episode, seeking medical attention is recommended to ensure appropriate care and evaluation of the underlying cause.
Medical Treatments and Interventions
While there are no specific medications designed to treat vasovagal syncope, certain medications may be prescribed to manage underlying conditions that contribute to the vasovagal response. Beta-blockers, for example, can help regulate heart rate and blood pressure. However, the decision to use medications should be made by a healthcare professional after a thorough evaluation of the individual’s medical history and symptom severity.
In addition to medications, non-pharmacological interventions can also be helpful in managing vasovagal syncope. Techniques such as applied tension, cognitive-behavioral therapy, and biofeedback have shown promise in reducing the frequency and severity of vasovagal episodes. Again, the implementation of these interventions should be guided by healthcare professionals.
Living with Vasovagal Syncope: Lifestyle Adjustments
Individuals living with vasovagal syncope can take certain lifestyle measures to minimize the occurrence of episodes and improve their overall well-being.
Diet and Hydration
Maintaining a balanced diet and staying properly hydrated can help regulate blood pressure and reduce the risk of vasovagal responses. Avoiding excessive consumption of stimulants like caffeine and alcohol may also be beneficial for some individuals. However, it is important to consult with a healthcare professional regarding any dietary modifications.
Exercise and Physical Activity
Regular exercise, under the guidance of a healthcare professional, can help improve cardiovascular health and decrease the likelihood of vasovagal responses. Engaging in activities that promote gentle, controlled movements, such as yoga or tai chi, may provide additional benefits for stress reduction.
Stress Management and Mental Health Care
Stress can exacerbate the vasovagal response, so developing effective stress management techniques is crucial. This may involve practicing relaxation exercises, seeking therapy or counseling, and adopting healthy coping strategies. Adequate sleep and maintaining a positive outlook can also contribute to overall well-being.
In conclusion, understanding the vasovagal response to needles is essential for both individuals and healthcare professionals alike. Recognizing the triggers, symptoms, and underlying causes of this response allows for improved management strategies and enhanced well-being. It is important to consult with a healthcare provider for personalized guidance and treatment options tailored to individual needs. By working together, we can make needle-related procedures more comfortable and safe for everyone.







Leave a Reply