Vasovagal constipation is a condition that affects the normal movement of the digestive system, leading to difficulty in bowel movements. By understanding its causes, symptoms, and treatment options, individuals can better manage this condition and improve their quality of life. It is important to note that while this article provides information, it is not a substitute for medical advice. Consulting with a healthcare professional is advised for an accurate diagnosis and personalized treatment plan.
What is Vasovagal Constipation?
Vasovagal constipation is a form of functional constipation. It occurs when there is an imbalance in the autonomic nervous system, particularly the vagus nerve. The vagus nerve plays a crucial role in regulating the muscles of the gastrointestinal tract, including the movement of stool through the intestines.
The Physiology Behind Vasovagal Constipation
In individuals with vasovagal constipation, the vagus nerve may be overly sensitive or impaired. This can result in disrupted signaling between the brain and the intestines, leading to delayed or ineffective bowel movements.
Common Misconceptions About Vasovagal Constipation
One common misconception is that vasovagal constipation is solely caused by diet or lack of physical activity. While these factors may contribute to the condition, it is a complex disorder with multifactorial causes.
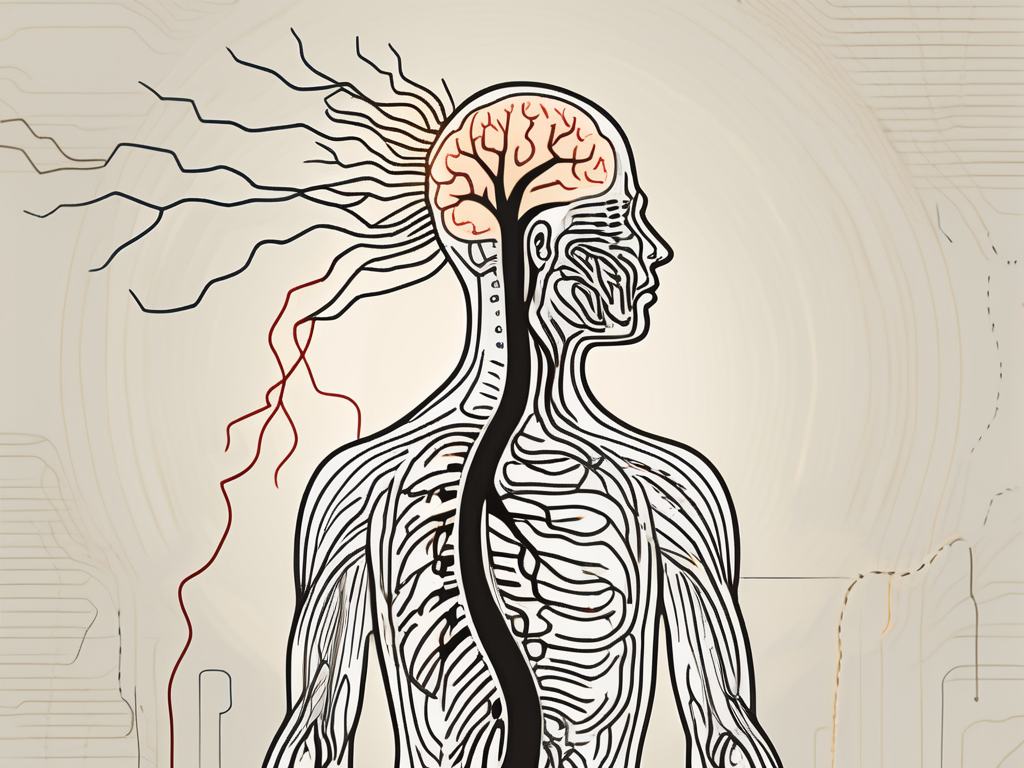
Understanding the Autonomic Nervous System
The autonomic nervous system is responsible for controlling involuntary bodily functions, such as heart rate, blood pressure, and digestion. It is divided into two branches: the sympathetic nervous system and the parasympathetic nervous system. The vagus nerve, also known as the tenth cranial nerve, is a major component of the parasympathetic nervous system and plays a crucial role in regulating gastrointestinal motility.
The Role of the Vagus Nerve in Gastrointestinal Function
The vagus nerve is responsible for transmitting signals between the brain and the gastrointestinal tract. It helps coordinate the contraction and relaxation of the muscles in the intestines, allowing for the smooth movement of food and waste through the digestive system. When the vagus nerve is functioning properly, it ensures that bowel movements occur at regular intervals and with appropriate force.
The Impact of Vagus Nerve Dysfunction
In individuals with vasovagal constipation, the vagus nerve may not be functioning optimally. This can lead to a variety of symptoms, including difficulty passing stool, infrequent bowel movements, and a feeling of incomplete evacuation. The disrupted signaling between the brain and the intestines can result in the muscles of the gastrointestinal tract not contracting effectively, leading to sluggish or ineffective movement of stool.
Factors Contributing to Vasovagal Constipation
While the exact causes of vasovagal constipation are not fully understood, several factors have been identified as potential contributors. These include genetic predisposition, hormonal imbalances, certain medications, stress, and underlying medical conditions such as irritable bowel syndrome (IBS) or neurological disorders.
The Importance of a Comprehensive Approach
Managing vasovagal constipation requires a comprehensive approach that takes into account the various factors that may be contributing to the condition. This may involve dietary modifications, increased physical activity, stress management techniques, and, in some cases, medication or other medical interventions. It is important for individuals with vasovagal constipation to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs.
Conclusion
Vasovagal constipation is a complex disorder that involves an imbalance in the autonomic nervous system, particularly the vagus nerve. Understanding the physiology behind vasovagal constipation and dispelling common misconceptions can help individuals better manage their condition and improve their quality of life. By taking a comprehensive approach to treatment, individuals can find relief from the symptoms of vasovagal constipation and regain control over their digestive health.
Identifying the Causes of Vasovagal Constipation
Lifestyle Factors Contributing to Vasovagal Constipation
Lifestyle factors play a significant role in the development or exacerbation of vasovagal constipation. One of the primary culprits is a sedentary lifestyle. Spending long hours sitting or engaging in minimal physical activity can lead to sluggish bowel movements. The lack of movement slows down the digestive process, making it harder for the intestines to push waste through the colon.
In addition to a sedentary lifestyle, inadequate fiber intake is another lifestyle factor that contributes to vasovagal constipation. Fiber is essential for maintaining regular bowel movements as it adds bulk to the stool, making it easier to pass. When there is a lack of fiber in the diet, the stool becomes hard and difficult to eliminate, leading to constipation.
Poor hydration is yet another lifestyle factor that can contribute to vasovagal constipation. When the body is dehydrated, the colon absorbs more water from the stool, making it dry and harder to pass. Drinking an adequate amount of water throughout the day helps keep the stool soft and promotes regular bowel movements.
Medical Conditions Associated with Vasovagal Constipation
Vasovagal constipation can also be associated with various medical conditions, further complicating the issue. One such condition is Parkinson’s disease, a neurological disorder that affects the movement of the muscles, including those responsible for bowel movements. The disrupted muscle coordination can lead to constipation in individuals with Parkinson’s disease.
Diabetes, another medical condition associated with vasovagal constipation, can affect the nerves that control the muscles in the digestive system. When these nerves are damaged or impaired due to diabetes, the normal rhythmic contractions necessary for proper bowel movements can be disrupted, resulting in constipation.
Multiple sclerosis, a chronic autoimmune disease that affects the central nervous system, can also contribute to vasovagal constipation. The damage to the nerves caused by multiple sclerosis can disrupt the communication between the brain and the intestines, leading to irregular bowel movements and constipation.
Thyroid dysfunction, such as hypothyroidism, can have a significant impact on bowel function. The thyroid hormone plays a crucial role in regulating the metabolism of the body, including the digestive system. When the thyroid hormone levels are imbalanced, it can slow down the digestive process, leading to constipation.
Managing these underlying medical conditions is crucial in improving bowel function for individuals with vasovagal constipation. Proper treatment and medication can help alleviate the symptoms and restore regularity to their digestive system.
Recognizing the Symptoms of Vasovagal Constipation
Physical Indicators of Vasovagal Constipation
Common physical symptoms of vasovagal constipation include infrequent bowel movements, straining during bowel movements, hard and dry stools, abdominal discomfort or pain, and a sense of incomplete evacuation.
When it comes to infrequent bowel movements, individuals with vasovagal constipation may find themselves going days without having a bowel movement. This can be frustrating and uncomfortable, as the body is not able to eliminate waste as efficiently as it should. The straining during bowel movements can also be a cause for concern, as it can lead to hemorrhoids or anal fissures.
Furthermore, the hard and dry stools that are characteristic of vasovagal constipation can make the act of passing stools incredibly painful. The stool may be difficult to pass, causing discomfort and even tears in the rectal area. This can result in bleeding and further complications.
Emotional and Psychological Symptoms
In addition to physical symptoms, individuals with vasovagal constipation may experience emotional and psychological symptoms, such as anxiety, depression, frustration, and decreased quality of life. It is important to address these aspects of the condition alongside the physical symptoms.
Anxiety can often accompany vasovagal constipation as individuals may worry about when their next bowel movement will occur or if they will experience pain during the process. This anxiety can further exacerbate the condition, as stress and tension can contribute to constipation.
Depression may also be a common emotional symptom experienced by those with vasovagal constipation. The frustration and discomfort caused by the condition can lead to feelings of sadness and hopelessness. It is important for individuals to seek support and treatment for both the physical and emotional aspects of vasovagal constipation.
Furthermore, the decreased quality of life experienced by individuals with vasovagal constipation cannot be overlooked. The condition can greatly impact daily activities and overall well-being. Simple tasks such as going to work or socializing with friends can become challenging and stressful due to the physical and emotional symptoms associated with vasovagal constipation.
Treatment Options for Vasovagal Constipation
Medical Interventions for Vasovagal Constipation
Treatment for vasovagal constipation may involve medication to regulate bowel movements or address underlying medical conditions. In some cases, the use of laxatives may be recommended to promote regularity. Laxatives work by softening the stool or stimulating bowel contractions, making it easier to pass. However, it is important to use laxatives under the guidance of a healthcare professional to avoid dependence or other side effects.
In addition to medication, procedures or surgeries may also be recommended in severe cases of vasovagal constipation. One such procedure is called a colonic transit study, which involves tracking the movement of food through the digestive system using X-rays. This can help identify any abnormalities or blockages that may be contributing to constipation. In some cases, surgery may be necessary to remove obstructions or repair damaged areas of the colon.
Consulting with a gastroenterologist or healthcare professional is crucial to determine the most appropriate treatment approach for vasovagal constipation. They will consider factors such as the severity of symptoms, underlying medical conditions, and individual preferences when developing a treatment plan.
Lifestyle Changes to Manage Vasovagal Constipation
Adopting certain lifestyle changes can also help manage vasovagal constipation. One of the most important changes is increasing fiber intake. Fiber adds bulk to the stool, making it easier to pass through the digestive system. Good sources of fiber include fruits, vegetables, whole grains, and legumes. It is recommended to gradually increase fiber intake to allow the body to adjust and prevent excessive gas or bloating.
In addition to fiber, staying adequately hydrated is essential for maintaining regular bowel movements. Drinking enough water helps soften the stool and prevent it from becoming hard and difficult to pass. Aim to drink at least eight glasses of water per day, and consider increasing intake during periods of physical activity or hot weather.
Engaging in regular physical activity can also help stimulate bowel movements and prevent constipation. Exercise promotes healthy digestion by increasing muscle contractions in the intestines. Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking or cycling, most days of the week.
Establishing a regular bowel routine is another important lifestyle change for managing vasovagal constipation. Try to set aside a specific time each day to sit on the toilet and attempt to have a bowel movement. This can help train the body to have regular and predictable bowel movements. It may also be helpful to create a relaxing environment in the bathroom, such as playing soft music or reading a book, to encourage relaxation and reduce stress.
It is advisable to work with a healthcare professional or registered dietitian to create an individualized plan for managing vasovagal constipation. They can provide guidance on dietary changes, recommend appropriate exercises, and monitor progress to ensure the most effective treatment approach.
Prevention Strategies for Vasovagal Constipation
Dietary Adjustments to Prevent Vasovagal Constipation
Avoiding processed foods is an essential step in preventing vasovagal constipation. Processed foods are often low in fiber and high in unhealthy fats, which can contribute to constipation. Instead, it is recommended to increase the consumption of fiber-rich foods such as fruits, vegetables, and whole grains. These foods provide essential nutrients and promote healthy bowel movements.
In addition to increasing fiber intake, ensuring an adequate fluid intake is crucial for preventing vasovagal constipation. Drinking enough water helps soften the stool and makes it easier to pass through the digestive system. It is recommended to drink at least eight glasses of water per day, but individual needs may vary.
Furthermore, managing any food intolerances or sensitivities can also contribute to improved bowel function. Some individuals may experience constipation as a result of certain foods that their bodies cannot tolerate. Identifying and avoiding these trigger foods can help prevent vasovagal constipation and promote overall digestive health.
Importance of Regular Exercise in Preventing Vasovagal Constipation
Engaging in regular physical activity has numerous benefits, including promoting proper bowel function. Exercise helps stimulate the gastrointestinal tract and promotes regular bowel movements. When we exercise, our muscles contract, including the muscles in the digestive system. This contraction helps move the stool through the intestines and prevents constipation.
It is important to note that individuals should consult with a healthcare professional before starting any exercise regimen, especially those with existing medical conditions. A healthcare professional can provide personalized advice and guidance on the most suitable exercises for preventing vasovagal constipation. They can also help determine the appropriate intensity and duration of exercise based on an individual’s overall health and fitness level.
In conclusion, making dietary adjustments and engaging in regular exercise are effective strategies for preventing vasovagal constipation. By adopting a fiber-rich diet, staying hydrated, and incorporating physical activity into daily routines, individuals can maintain healthy bowel function and reduce the risk of constipation. It is important to prioritize digestive health and seek professional guidance when necessary to ensure the most appropriate prevention strategies are implemented.
Living with Vasovagal Constipation
Coping Mechanisms for Vasovagal Constipation
Vasovagal constipation can significantly impact an individual’s quality of life. Developing coping mechanisms, such as practicing relaxation techniques, engaging in stress management activities, and seeking emotional support, can help individuals better manage the emotional and psychological aspects of the condition.
Living with vasovagal constipation can be challenging, but individuals are not alone. Connecting with support groups or seeking professional help, such as counseling or therapy, can provide valuable guidance and support. It is important to reach out to healthcare professionals for any concerns related to vasovagal constipation.
One coping mechanism that individuals with vasovagal constipation can practice is deep breathing exercises. Deep breathing helps to relax the body and reduce stress levels, which can in turn alleviate constipation symptoms. By taking slow, deep breaths and focusing on the inhalation and exhalation, individuals can promote a sense of calm and relaxation.
In addition to deep breathing exercises, engaging in regular physical activity can also be beneficial for managing vasovagal constipation. Exercise helps to stimulate the muscles in the digestive system, promoting bowel movements and preventing constipation. Whether it’s going for a walk, practicing yoga, or participating in a sport, finding an activity that is enjoyable and suits one’s physical abilities can make a significant difference in managing the condition.
Furthermore, incorporating dietary changes can also play a role in managing vasovagal constipation. Increasing fiber intake by consuming more fruits, vegetables, whole grains, and legumes can help soften the stool and promote regular bowel movements. It is important to drink plenty of water as well, as dehydration can worsen constipation symptoms.
Seeking emotional support is another important aspect of coping with vasovagal constipation. Talking to friends, family, or joining support groups can provide individuals with a safe space to share their experiences, frustrations, and concerns. Connecting with others who are going through similar challenges can provide a sense of understanding and validation, as well as offer practical advice and coping strategies.
It is crucial to remember that managing vasovagal constipation is a journey, and what works for one person may not work for another. Therefore, it is important to explore different coping mechanisms and find a combination of strategies that work best for each individual. With time, patience, and support, individuals can learn to effectively manage vasovagal constipation and improve their overall well-being.
In conclusion, understanding vasovagal constipation is crucial for managing the condition effectively. By identifying the causes, recognizing the symptoms, exploring treatment options, and implementing prevention strategies, individuals can improve their bowel function and overall well-being. Remember, this article is not a replacement for medical advice. Consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.




Leave a Reply