Vasovagal syncope is a common condition that affects millions of people worldwide. It is characterized by a sudden loss of consciousness, often accompanied by a brief period of lightheadedness or dizziness. While the exact cause of vasovagal syncope is not fully understood, it is believed to be due to a temporary disruption of blood flow to the brain. In this article, we will explore the causes, symptoms, and treatment options for vasovagal syncope, with a particular focus on the role of swallowing in triggering this condition.
What is Vasovagal Syncope?
Vasovagal syncope, also known as neurocardiogenic syncope, is a type of fainting episode that occurs when there is a sudden drop in blood pressure and heart rate. This drop in blood flow to the brain leads to a temporary loss of consciousness. Vasovagal syncope is often triggered by certain factors, such as stress, pain, fear, or standing for long periods of time.
The Role of the Vagus Nerve in the Body
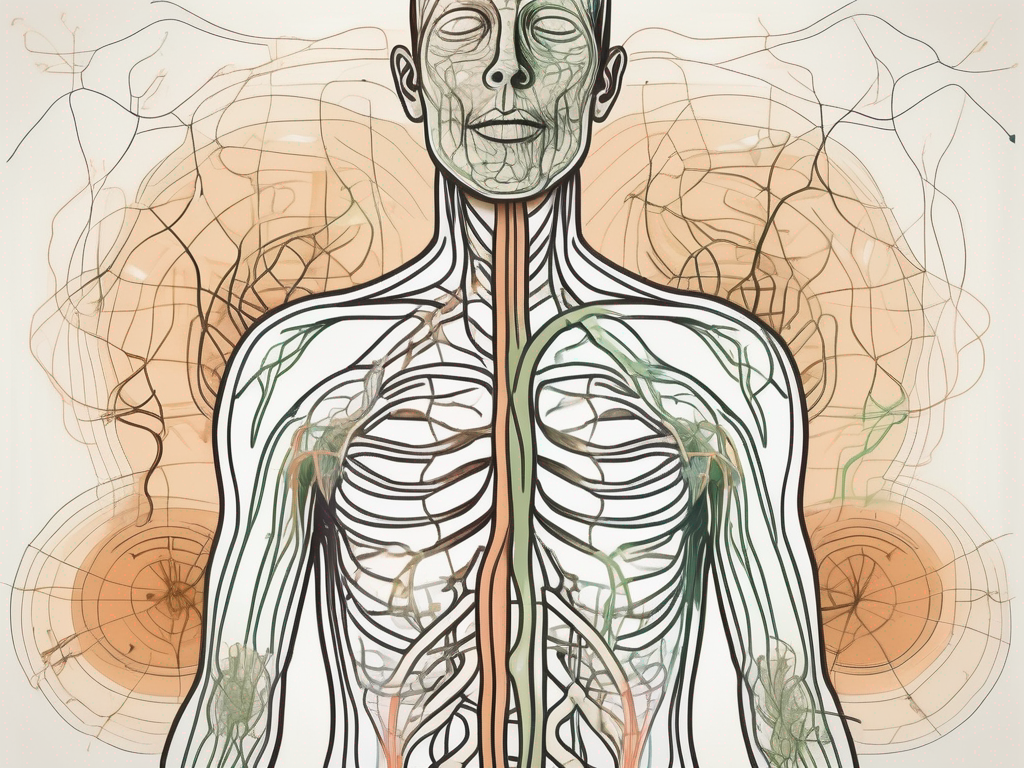
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, digestion, and swallowing. It is responsible for transmitting signals between the brain and different parts of the body. The vagus nerve has both sensory and motor functions and is essential for maintaining overall physiological balance.
The vagus nerve originates in the medulla oblongata, which is located in the brainstem. It extends down through the neck and chest, branching out to various organs and tissues in the body. This extensive network allows the vagus nerve to communicate with different systems, ensuring their proper functioning.
One of the key functions of the vagus nerve is to regulate heart rate. It acts as a natural pacemaker, sending electrical signals to the heart to control its rhythm. When the vagus nerve is activated, it slows down the heart rate, promoting relaxation and reducing stress. This is why techniques such as deep breathing and meditation, which stimulate the vagus nerve, are often used to calm the body and mind.
The Connection Between the Vagus Nerve and Fainting
Vasovagal syncope is thought to occur due to an overstimulation of the vagus nerve. When certain triggers, such as emotional stress or sudden pain, activate the vagus nerve, it can cause a reflex response that leads to a drop in blood pressure and heart rate. This, in turn, reduces blood flow to the brain, resulting in fainting.
During a vasovagal syncope episode, the vagus nerve sends signals to the heart, instructing it to slow down and dilate blood vessels. This causes a sudden decrease in blood pressure, which can lead to dizziness, lightheadedness, and ultimately, loss of consciousness. The body’s natural response to this drop in blood pressure is to lie down, allowing blood to flow more easily to the brain and prevent further fainting episodes.
It is important to note that vasovagal syncope is a temporary condition and does not typically cause any long-term harm. However, it can be a cause for concern, especially if it occurs frequently or without any apparent triggers. In such cases, medical evaluation and treatment may be necessary to identify and address any underlying causes or contributing factors.
Managing vasovagal syncope often involves identifying and avoiding triggers that may lead to fainting episodes. This may include practicing stress-reduction techniques, maintaining a healthy lifestyle, and staying well-hydrated. In some cases, medications or other interventions may be prescribed to help regulate blood pressure and prevent syncope.
Overall, understanding the role of the vagus nerve in vasovagal syncope can provide valuable insights into this common condition. By recognizing the connection between triggers, the vagus nerve, and fainting episodes, individuals can take steps to manage and minimize the impact of vasovagal syncope on their daily lives.
Swallowing and Its Impact on Vasovagal Syncope
Surprisingly, swallowing can also trigger vasovagal syncope in some individuals. The act of swallowing involves the coordination of various muscles and nerves in the throat and esophagus. This process can stimulate the vagus nerve, leading to a reflex response that may result in fainting.
When we think of swallowing, we often associate it with the simple act of moving food or liquid from our mouths to our stomachs. However, the physiology of swallowing is much more intricate than meets the eye. It is a complex process that involves the sequential contraction and relaxation of muscles in the mouth, throat, and esophagus.
Let’s dive deeper into the fascinating journey that food or liquid takes as it makes its way through our bodies. It all begins with the voluntary movement of the substance into the mouth. As we chew and mix it with saliva, the muscles in our mouth and tongue work together to form a cohesive bolus.
Once the bolus is ready, the swallowing process kicks into gear. The tongue pushes the bolus toward the back of the throat, triggering the opening of the upper esophageal sphincter. This sphincter allows the bolus to enter the esophagus, the muscular tube that connects the throat to the stomach.
As the bolus moves down the esophagus, a series of coordinated muscle contractions called peristalsis propels it forward. This rhythmic squeezing action ensures that the bolus reaches its destination – the stomach. It’s important to note that once the swallowing process begins, it becomes involuntary, meaning we cannot consciously control it.
So, how does swallowing relate to vasovagal syncope? Well, the answer lies in the intricate network of nerves that are involved in the swallowing process. One of the key players is the vagus nerve, also known as the tenth cranial nerve.
The vagus nerve plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, and digestion. It is responsible for transmitting signals between the brain and the organs in the chest and abdomen. When it comes to swallowing, the vagus nerve is activated to coordinate the complex muscle movements required for this process.
For some individuals, this activation of the vagus nerve during swallowing can have unintended consequences. It can trigger a reflex response that leads to a sudden drop in blood pressure, also known as vasovagal syncope. This drop in blood pressure can result in fainting or loss of consciousness.
Although the exact mechanism behind this phenomenon is not fully understood, researchers believe that the stimulation of the vagus nerve during swallowing somehow disrupts the normal balance of the autonomic nervous system. This disruption can cause a sudden decrease in heart rate and blood pressure, leading to vasovagal syncope.
It’s important to note that not everyone experiences vasovagal syncope when they swallow. This phenomenon seems to affect only a subset of individuals who may have a heightened sensitivity or predisposition to vagal reflexes. Further research is needed to fully unravel the complexities of this intriguing connection between swallowing and vasovagal syncope.
Identifying the Symptoms of Vasovagal Syncope
Vasovagal syncope can manifest through a variety of symptoms, which can differ from person to person. It is essential to recognize these symptoms to seek appropriate medical attention and rule out any underlying health conditions that may be causing the fainting episodes.
When it comes to vasovagal syncope, the symptoms can be quite diverse. While some individuals may experience a sudden loss of consciousness, others may only experience pre-syncopal symptoms without completely losing consciousness. It is important to note that these symptoms can be alarming and may cause distress, but they are usually not life-threatening.
Physical Symptoms
The physical symptoms of vasovagal syncope may include dizziness, lightheadedness, blurred vision, pale skin, sweating, and a slow heart rate. These symptoms often occur as a result of a sudden drop in blood pressure and a decrease in heart rate. The body’s autonomic nervous system, responsible for regulating involuntary bodily functions, can become overactive, leading to these physical manifestations.
Dizziness is a common symptom experienced by individuals with vasovagal syncope. It is characterized by a sensation of lightheadedness or feeling unsteady on one’s feet. Blurred vision may also occur, making it difficult to focus or see clearly. Additionally, the skin may appear pale due to reduced blood flow to the surface of the body. Sweating is another common symptom, as the body tries to regulate its temperature during a fainting episode. Lastly, a slow heart rate, known as bradycardia, can be observed during vasovagal syncope.
Emotional and Cognitive Symptoms
In addition to physical symptoms, vasovagal syncope can also lead to emotional and cognitive changes. Some people may feel anxious, confused, or have difficulty concentrating before or after a fainting episode. These symptoms are temporary and usually resolve once the underlying cause is addressed.
The emotional and cognitive symptoms experienced during vasovagal syncope can be attributed to the body’s response to the sudden drop in blood pressure. The brain may receive inadequate blood flow, leading to temporary changes in mood and cognitive function. Anxiety and confusion are common emotional symptoms, often caused by the fear and uncertainty associated with fainting episodes. Difficulty concentrating may also occur, making it challenging to focus on tasks or remember details.
It is important to note that while vasovagal syncope can be disruptive and distressing, it is typically a benign condition. However, if you experience frequent fainting episodes or have concerns about your symptoms, it is crucial to consult a healthcare professional for a proper diagnosis and appropriate management.
Causes of Vasovagal Syncope
There are several factors that can trigger or contribute to the occurrence of vasovagal syncope. These triggers can differ from person to person, and it is essential to identify and avoid them where possible. It is important to note that vasovagal syncope is not a life-threatening condition, but it can significantly impact an individual’s quality of life.
Common Triggers for Vasovagal Syncope
Some common triggers for vasovagal syncope include emotional stress, pain, fear, prolonged standing or sitting, intense physical activity, sudden changes in posture, and exposure to hot or crowded environments. Identifying and managing these triggers can help reduce the frequency of fainting episodes.
Emotional stress can be a significant trigger for vasovagal syncope. When a person experiences intense emotions such as anxiety, fear, or anger, it can lead to a sudden drop in blood pressure and heart rate, resulting in fainting. It is crucial for individuals prone to vasovagal syncope to find healthy ways to manage their stress levels, such as practicing relaxation techniques or seeking therapy.
Pain, whether acute or chronic, can also trigger vasovagal syncope. When the body experiences pain, it can activate the vagus nerve, which plays a role in regulating heart rate and blood pressure. This activation can lead to a vasovagal response, causing a person to faint. Proper pain management strategies, such as medication or physical therapy, can help minimize the risk of syncope episodes.
Prolonged standing or sitting in one position can cause blood to pool in the lower extremities, leading to a drop in blood pressure and subsequent fainting. This is particularly common in situations where individuals are not able to move or shift their weight, such as during long flights or extended periods of standing at work. Taking regular breaks to stretch, staying hydrated, and wearing compression stockings can help alleviate this trigger.
Intense physical activity can also induce vasovagal syncope, especially if the body is not adequately prepared or conditioned for the exertion. When engaging in vigorous exercise, the body requires increased blood flow to meet the demands of the muscles. However, in individuals prone to vasovagal syncope, this increased demand can overwhelm the body’s ability to maintain blood pressure, resulting in fainting. Gradually building up endurance and staying hydrated during exercise can help prevent syncope episodes.
Sudden changes in posture, such as standing up quickly or bending over, can trigger vasovagal syncope. These movements can cause a rapid redistribution of blood in the body, leading to a temporary drop in blood pressure. Individuals with vasovagal syncope may need to be cautious when changing positions and take their time to allow their body to adjust gradually.
Exposure to hot or crowded environments can also contribute to vasovagal syncope. High temperatures can cause blood vessels to dilate, leading to a drop in blood pressure. Additionally, being in a crowded space can increase anxiety and stress levels, further exacerbating the risk of fainting. It is important for individuals with vasovagal syncope to stay hydrated, avoid excessive heat exposure, and find ways to stay cool in crowded situations.
Underlying Health Conditions
Vasovagal syncope can also be associated with underlying health conditions, such as heart problems, dehydration, medication side effects, certain neurological disorders, and blood sugar imbalances. It is crucial to consult with a healthcare professional to rule out any potential underlying causes of vasovagal syncope.
Heart problems, such as arrhythmias or structural abnormalities, can disrupt the normal functioning of the cardiovascular system, leading to vasovagal syncope. It is important for individuals experiencing syncope episodes to undergo thorough cardiac evaluations to identify any underlying heart conditions that may require treatment or management.
Dehydration can also contribute to vasovagal syncope. When the body does not have enough fluids, it can lead to a decrease in blood volume, causing a drop in blood pressure. Ensuring adequate hydration by drinking enough water throughout the day is essential for individuals prone to syncope episodes.
Medications, particularly those that affect blood pressure or heart rate, can have side effects that increase the risk of vasovagal syncope. It is important for individuals taking medications to discuss potential side effects with their healthcare provider and adjust their treatment plan if necessary.
Certain neurological disorders, such as epilepsy or autonomic dysfunction, can be associated with vasovagal syncope. These conditions can affect the normal regulation of the autonomic nervous system, which plays a role in controlling heart rate and blood pressure. Proper diagnosis and management of these underlying neurological conditions are crucial in reducing the occurrence of syncope episodes.
Blood sugar imbalances, such as low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia), can also trigger vasovagal syncope. When blood sugar levels are not within the normal range, it can disrupt the body’s ability to maintain stable blood pressure. Individuals with diabetes or other conditions that affect blood sugar levels should work closely with their healthcare team to ensure proper management and minimize the risk of syncope.
Diagnosis of Vasovagal Syncope
Diagnosing vasovagal syncope involves a comprehensive evaluation of the individual’s medical history, physical examination, and specific diagnostic tests. A healthcare professional will carefully assess the symptoms and triggers to develop an accurate diagnosis and recommend appropriate treatment strategies.
Medical History and Physical Examination
During the medical history assessment, the healthcare professional will ask questions regarding the individual’s symptoms, triggers, and any previous medical conditions. They will also perform a thorough physical examination to assess vital signs, heart function, and neurological responses.
Diagnostic Tests and Procedures
In some cases, additional diagnostic tests may be required to confirm the diagnosis of vasovagal syncope and rule out other potential causes. These tests may include an electrocardiogram (ECG) to evaluate heart rhythm, a tilt table test to trigger fainting episodes in a controlled environment, or blood tests to check for any underlying abnormalities.
Treatment Options for Vasovagal Syncope
While there is no specific cure for vasovagal syncope, several treatment options are available to help manage and reduce the frequency of fainting episodes. The optimal treatment approach will depend on the individual’s symptoms, triggers, and overall health status.
Lifestyle Changes and Home Remedies
Making certain lifestyle modifications can significantly help manage vasovagal syncope. It is recommended to avoid triggers, such as emotional stress, prolonged standing, intense physical activity, and exposure to extreme temperatures. Staying hydrated, maintaining a balanced diet, and getting regular exercise can also have a positive impact on overall cardiovascular health. It is important to consult with a healthcare professional to determine the most appropriate lifestyle modifications for individual needs.
Medications and Therapies
In some cases, medications may be prescribed to control the occurrence and severity of vasovagal syncope episodes. These medications may include beta-blockers to regulate heart rate and blood pressure, or other medications that target specific underlying causes or triggers. In addition to medications, certain therapies, such as biofeedback or cognitive-behavioral therapy, may be recommended to help manage stress and anxiety, which can contribute to vasovagal syncope.
Surgical Interventions
In rare cases when conservative treatments are ineffective, surgical interventions may be considered. These interventions may include the insertion of a pacemaker or other devices that help regulate heart rhythm and prevent fainting. Surgical options should be thoroughly discussed with a healthcare professional, considering the potential risks and benefits.
Living with Vasovagal Syncope
Vasovagal syncope can be challenging to manage, but with appropriate medical care and self-care strategies, individuals can lead fulfilling lives. It is important to focus on self-awareness and recognize the triggers that may lead to fainting. Coping strategies, such as deep breathing exercises, staying well-hydrated, and maintaining good overall health, can help minimize the impact of vasovagal syncope on daily activities.
Coping Strategies and Support
Developing coping strategies can significantly improve the management of vasovagal syncope. These strategies may include practicing relaxation techniques, such as deep breathing or meditation, avoiding triggers, and adopting a healthy lifestyle. Additionally, seeking support from healthcare professionals, support groups, or online communities can provide valuable information and emotional support for individuals living with vasovagal syncope.
Prognosis and Long-term Management
With appropriate medical care and lifestyle modifications, the prognosis for individuals with vasovagal syncope is generally good. While the condition may persist, most people experience a reduction in the frequency and severity of fainting episodes over time. It is crucial to maintain regular follow-ups with a healthcare professional to monitor any changes in symptoms and adjust the treatment plan accordingly.
In conclusion, understanding vasovagal syncope and its relationship with swallowing can shed light on this common condition. By recognizing the triggers, symptoms, and treatment options, individuals can take proactive steps to manage vasovagal syncope and improve their overall quality of life. It is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.







Leave a Reply