Convulsive Vasovagal Syncope is a condition that involves a sudden loss of consciousness and muscle control due to a temporary decrease in blood flow to the brain. It is a type of fainting spell that is characterized by convulsive movements and is usually triggered by certain factors. In this article, we will delve into the various aspects of Convulsive Vasovagal Syncope, including its definition, underlying causes, symptoms, diagnosis, and available treatment options.
What is Convulsive Vasovagal Syncope?
Convulsive Vasovagal Syncope, also known as neurocardiogenic syncope or reflex syncope, is a common type of fainting episode. It occurs when there is a sudden drop in heart rate and blood pressure, leading to a temporary disruption of blood supply to the brain. Unlike other types of syncope, convulsive vasovagal syncope is characterized by the presence of convulsive movements during the event, which can be mistaken for a seizure.
Defining Convulsive Vasovagal Syncope
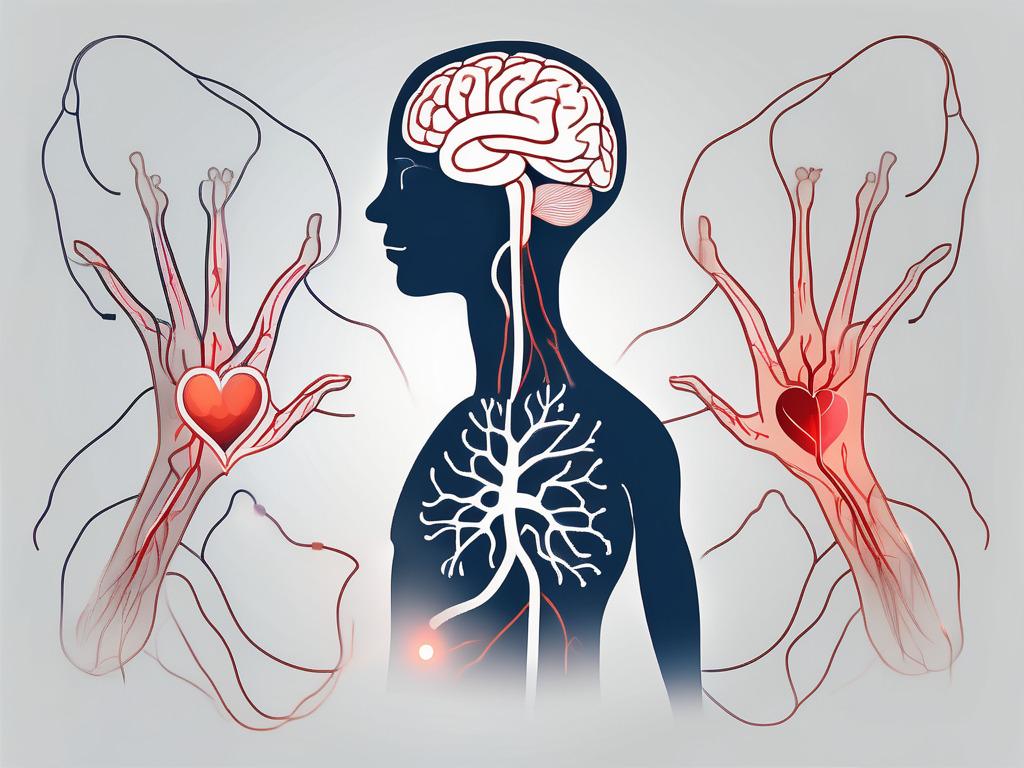
Convulsive Vasovagal Syncope is a reflex-mediated response that is triggered by various factors, such as emotional distress, pain, prolonged standing, or blood phobia. The precise mechanism behind this condition involves a stimulation of the vagus nerve, which leads to a sudden slowing of the heart rate and a drop in blood pressure. This ultimately results in a transient loss of consciousness and muscle control.
The Physiology Behind Convulsive Vasovagal Syncope
During a convulsive vasovagal syncope episode, the autonomic nervous system, which controls involuntary bodily functions, becomes overactive. This triggers a series of physiological responses, including a sudden constriction of blood vessels and a decrease in heart rate. As a result, blood flow to the brain diminishes, causing the individual to lose consciousness.
When it comes to emotional distress as a trigger for convulsive vasovagal syncope, it is important to understand that the brain and the heart are closely interconnected. The brain sends signals to the heart through the autonomic nervous system, which regulates heart rate and blood pressure. In times of extreme emotional stress, such as fear or anxiety, the brain can send signals that disrupt the normal functioning of the autonomic nervous system, leading to a fainting episode.
Pain, another common trigger for convulsive vasovagal syncope, can also have a profound impact on the body’s physiological responses. When an individual experiences intense pain, the body releases stress hormones, such as adrenaline, which can cause a sudden increase in heart rate and blood pressure. However, in some cases, the body’s response to pain can be the opposite, resulting in a drop in heart rate and blood pressure, leading to a fainting episode.
Prolonged standing is yet another trigger for convulsive vasovagal syncope. When a person stands for an extended period of time, gravity causes blood to pool in the lower extremities. This pooling of blood can lead to a decrease in blood flow to the brain, resulting in a fainting episode. Additionally, standing for long periods can also put strain on the leg muscles, which can activate the autonomic nervous system and trigger a reflex response that leads to syncope.
Blood phobia, or the fear of blood, is a unique trigger for convulsive vasovagal syncope. When an individual with blood phobia is exposed to blood or the sight of blood, it can trigger a strong emotional response. This emotional response can activate the autonomic nervous system, leading to a sudden drop in heart rate and blood pressure, and ultimately causing a fainting episode.
Understanding the physiology behind convulsive vasovagal syncope is crucial in managing and preventing future episodes. By identifying triggers and implementing strategies to avoid or manage them, individuals with this condition can lead a more comfortable and confident life.
Causes of Convulsive Vasovagal Syncope
The exact causes of Convulsive Vasovagal Syncope are not fully understood. However, there are several factors that can contribute to the occurrence of fainting episodes:
Genetic Factors
Research suggests that certain individuals may have a genetic predisposition to developing convulsive vasovagal syncope. It is believed that certain genetic variations may affect the regulation of the autonomic nervous system, making them more susceptible to fainting episodes.
Genetic studies have shown that specific gene mutations can disrupt the normal functioning of the autonomic nervous system, leading to an increased risk of convulsive vasovagal syncope. These mutations can affect the production or activity of neurotransmitters involved in regulating blood pressure and heart rate. Understanding the genetic basis of this condition can help in developing targeted therapies and interventions.
Furthermore, family history plays a significant role in determining an individual’s susceptibility to convulsive vasovagal syncope. If a close family member has experienced fainting episodes, there is a higher likelihood of developing the condition.
Environmental Triggers
Various environmental triggers can precipitate convulsive vasovagal syncope in susceptible individuals. These triggers can include emotional stress, pain, the sight of blood, prolonged standing, and hot or crowded environments. Understanding these triggers can help patients identify and manage their episodes.
Emotional stress, such as anxiety or fear, can activate the body’s fight-or-flight response, leading to a sudden drop in blood pressure and fainting. Similarly, the sight of blood or experiencing pain can trigger a vasovagal response, causing a temporary loss of consciousness.
Prolonged standing can result in blood pooling in the lower extremities, leading to decreased blood flow to the brain and fainting. Hot or crowded environments can also contribute to fainting episodes by causing dehydration, vasodilation, and an overall increase in physiological stress.
Identifying and avoiding these triggers can significantly reduce the frequency and severity of convulsive vasovagal syncope episodes. Patients are often advised to practice stress management techniques, maintain proper hydration, and avoid prolonged periods of standing or exposure to extreme temperatures.
Underlying Medical Conditions
Convulsive Vasovagal Syncope can also occur as a result of underlying medical conditions. These can include heart rhythm disorders, structural heart abnormalities, autonomic nervous system disorders, or hormonal imbalances. It is important to identify and treat these underlying conditions, as they can contribute to the frequency and severity of the fainting episodes.
Heart rhythm disorders, such as bradycardia (slow heart rate) or tachycardia (fast heart rate), can disrupt the normal electrical signals that regulate the heartbeat. This can lead to inadequate blood flow to the brain and fainting episodes.
Structural heart abnormalities, such as valve defects or congenital heart diseases, can affect the heart’s ability to pump blood efficiently. This can result in reduced blood flow to the brain, triggering fainting episodes.
Autonomic nervous system disorders, such as dysautonomia or postural orthostatic tachycardia syndrome (POTS), can disrupt the normal regulation of blood pressure and heart rate. These conditions can increase the risk of vasovagal syncope and convulsive episodes.
Hormonal imbalances, particularly in conditions like Addison’s disease or pheochromocytoma, can affect blood pressure regulation and contribute to fainting episodes.
Diagnosing and managing these underlying medical conditions is crucial in effectively managing convulsive vasovagal syncope. Treatment options may include medication to regulate heart rhythm, surgical interventions to correct structural abnormalities, or hormone replacement therapy to restore hormonal balance.
Expanding our understanding of the causes of convulsive vasovagal syncope is essential for developing targeted treatments and improving the quality of life for individuals affected by this condition. Ongoing research aims to uncover additional genetic, environmental, and physiological factors that contribute to the development and progression of convulsive vasovagal syncope.
Recognizing the Symptoms of Convulsive Vasovagal Syncope
Convulsive Vasovagal Syncope is characterized by a specific set of symptoms, which can vary from person to person. Recognizing these symptoms is crucial in differentiating convulsive vasovagal syncope from other conditions:
During a convulsive vasovagal syncope episode, individuals may experience a sudden feeling of lightheadedness, dizziness, or nausea. This can be accompanied by a variety of physical symptoms that are indicative of the condition. For example, they may notice a pale complexion, sweating, and a slow, weak pulse. These physical manifestations can often be alarming and may cause individuals to seek medical attention.
In addition to the physical symptoms, convulsive movements, such as jerking or tremors, may also occur during a convulsive vasovagal syncope episode. These movements can be mistaken for a seizure, leading to further confusion and concern. It is important for individuals and healthcare professionals to be aware of this distinction in order to provide appropriate care and treatment.
Convulsive Vasovagal Syncope can also lead to emotional and cognitive symptoms. In some cases, individuals may experience anxiety, fear, confusion, or a sense of impending doom prior to fainting. These emotional and cognitive symptoms can be distressing and often contribute to the overall subjective experience of the condition. Understanding and addressing these symptoms can play a crucial role in managing convulsive vasovagal syncope.
It is worth noting that the presentation of convulsive vasovagal syncope can vary across different age groups. For instance, in younger individuals, episodes may be more commonly triggered by emotional stress or pain. This highlights the importance of considering age-related factors when diagnosing and treating convulsive vasovagal syncope. On the other hand, in older adults, episodes may be more associated with orthostatic stress, such as standing up too quickly. Recognizing these age-related patterns can aid in providing targeted interventions and support.
Diagnosing Convulsive Vasovagal Syncope
Diagnosing Convulsive Vasovagal Syncope requires a thorough evaluation of the patient’s medical history, a physical examination, and the appropriate diagnostic tests. The goal is to rule out other possible causes for the symptoms and determine if the episodes are indeed due to convulsive vasovagal syncope:
Medical History and Physical Examination
A detailed medical history and physical examination can provide valuable clues regarding the underlying cause of the fainting episodes. The healthcare provider will ask about the symptoms, triggers, and frequency of the episodes. They will also assess the patient’s vital signs, neurological function, and cardiovascular health.
During the medical history assessment, the healthcare provider will inquire about any previous medical conditions, family history of fainting episodes, and any medications the patient may be taking. This information can help identify any potential risk factors or underlying conditions that may contribute to the development of convulsive vasovagal syncope.
The physical examination will involve a comprehensive assessment of the patient’s overall health. The healthcare provider will check the patient’s blood pressure, heart rate, and rhythm. They will also perform a neurological examination to evaluate the patient’s reflexes, coordination, and sensory function. Additionally, the cardiovascular system will be examined to identify any abnormalities or signs of underlying heart disease.
Diagnostic Tests and Procedures
In some cases, additional diagnostic tests may be necessary to confirm the diagnosis of convulsive vasovagal syncope. These tests can include an electrocardiogram (ECG) to evaluate the heart’s electrical activity, a tilt table test to provoke and assess the patient’s response to certain triggers, or an echocardiogram to examine the heart’s structure and function.
The electrocardiogram (ECG) is a non-invasive test that records the electrical activity of the heart. It can help identify any abnormal heart rhythms or conduction abnormalities that may contribute to the fainting episodes. The tilt table test involves placing the patient on a table that can be tilted to different angles. This test helps provoke fainting episodes and allows healthcare providers to observe the patient’s response, helping to confirm the diagnosis of convulsive vasovagal syncope.
An echocardiogram is a test that uses sound waves to create images of the heart. It provides detailed information about the heart’s structure and function, allowing healthcare providers to assess for any structural abnormalities or underlying heart disease that may be causing the fainting episodes.
Differential Diagnosis
It is crucial to differentiate convulsive vasovagal syncope from other conditions that can cause similar symptoms, such as seizures, heart arrhythmias, or underlying structural heart abnormalities. This requires a comprehensive evaluation by a healthcare professional who specializes in the diagnosis and management of fainting disorders.
During the differential diagnosis process, the healthcare provider will consider other potential causes for the fainting episodes and may order additional tests or consultations with specialists. This may include neurologists, cardiologists, or electrophysiologists who can provide expertise in evaluating and managing conditions that can mimic convulsive vasovagal syncope.
The healthcare provider will carefully review the patient’s medical history, physical examination findings, and the results of any diagnostic tests to make an accurate diagnosis. They will also take into account the patient’s symptoms, triggers, and response to treatment, if any, to ensure an appropriate management plan is developed.
Treatment Options for Convulsive Vasovagal Syncope
The treatment of Convulsive Vasovagal Syncope focuses on preventing the occurrence of fainting episodes and managing the underlying triggers and contributing factors. The specific treatment approach will depend on the individual patient and the severity of the condition:
Lifestyle Changes and Home Remedies
For some individuals, making certain lifestyle modifications and adopting home remedies can help reduce the frequency and severity of convulsive vasovagal syncope episodes. These may include avoiding known triggers, maintaining proper hydration, maintaining a healthy diet, and practicing stress reduction techniques, such as meditation or deep breathing exercises.
In addition to these lifestyle changes, it is important for individuals with convulsive vasovagal syncope to prioritize self-care. This may involve getting enough sleep, engaging in regular physical activity, and managing stress levels. By taking care of their overall well-being, individuals can potentially reduce the likelihood of experiencing fainting episodes.
Medication and Therapies
In certain cases, medications may be prescribed to help manage the symptoms and prevent fainting episodes. These medications may include beta-blockers, which help regulate heart rate and blood pressure, or selective serotonin reuptake inhibitors (SSRIs), which can help manage associated anxiety or depression.
It is important to note that medication should always be prescribed and monitored by a healthcare professional, as they will determine the appropriate dosage and duration of treatment based on the individual’s specific needs. Additionally, therapies such as biofeedback or cognitive-behavioral therapy may be beneficial in some cases.
Furthermore, individuals with convulsive vasovagal syncope may find it helpful to explore alternative therapies, such as acupuncture or herbal remedies. While the effectiveness of these treatments may vary from person to person, some individuals have reported positive results in managing their symptoms through these approaches.
Surgical Interventions
For individuals with severe and refractory convulsive vasovagal syncope, surgical interventions may be considered. These interventions, such as pacemaker implantation or sympathetic denervation, aim to modulate the autonomic nervous system and improve heart rate regulation.
Pacemaker implantation involves the surgical placement of a small device that helps regulate the heart’s electrical activity. This can be particularly beneficial for individuals whose fainting episodes are triggered by bradycardia, a condition characterized by an abnormally slow heart rate.
Sympathetic denervation, on the other hand, involves the surgical interruption of certain nerve pathways that are responsible for regulating blood pressure and heart rate. By disrupting these pathways, the excessive activation of the autonomic nervous system can be reduced, potentially leading to a decrease in fainting episodes.
It is important to note that surgical interventions are typically reserved for select cases and should be discussed with a healthcare professional. The decision to undergo surgery should be carefully considered, weighing the potential benefits against the risks and potential complications associated with the procedure.
In conclusion, the treatment options for convulsive vasovagal syncope are diverse and depend on the individual patient’s needs and the severity of the condition. Lifestyle changes, medication, therapies, and surgical interventions all play a role in managing and preventing fainting episodes. It is crucial for individuals with convulsive vasovagal syncope to work closely with their healthcare team to develop a personalized treatment plan that addresses their specific needs and improves their overall quality of life.
Living with Convulsive Vasovagal Syncope
Coping with Convulsive Vasovagal Syncope can be challenging, but with proper management and support, individuals can lead fulfilling lives:
Coping Strategies and Support
Implementing coping strategies can help individuals better manage convulsive vasovagal syncope and its associated challenges. These strategies may include learning relaxation techniques, carrying medical identification, and informing family, friends, and coworkers about the condition. Additionally, seeking support from patient advocacy groups or support groups can provide individuals with valuable emotional support and a sense of community.
Prognosis and Long-Term Management
The prognosis for individuals with convulsive vasovagal syncope is generally favorable. With proper diagnosis, treatment, and lifestyle modifications, most individuals can effectively manage their symptoms and prevent fainting episodes. Regular follow-ups with a healthcare professional are essential to monitor the condition’s progression and make any necessary adjustments to the treatment plan.
Preventing Recurrence and Complications
Preventing the recurrence of convulsive vasovagal syncope episodes is a key aspect of long-term management. This involves identifying and avoiding triggers, managing underlying medical conditions, and adhering to the prescribed treatment plan. If complications, such as injuries resulting from falls during episodes, occur, appropriate medical attention should be sought.
In conclusion, understanding Convulsive Vasovagal Syncope is essential for individuals living with this condition and their healthcare providers. By recognizing its causes, symptoms, and available treatment options, individuals can effectively manage their symptoms, improve their quality of life, and minimize the occurrence of fainting episodes. It is important to consult with a healthcare professional for a proper diagnosis and to develop an individualized treatment plan tailored to personal needs and circumstances.





Leave a Reply