When it comes to understanding the intricacies of our body, one area of interest lies in the connection between vasovagal syncope and anxiety. Vasovagal syncope, often referred to as fainting, is a sudden loss of consciousness caused by a decrease in blood flow to the brain. Anxiety, on the other hand, is a complex mental health condition characterized by excessive worry and fear. While seemingly unrelated, research suggests a correlation between these two phenomena. In this article, we will delve into the defining characteristics of vasovagal syncope and anxiety, explore their intersection, examine new medical research on the connection, discuss treatment approaches, and provide insights on living with these conditions.
Defining Vasovagal Syncope
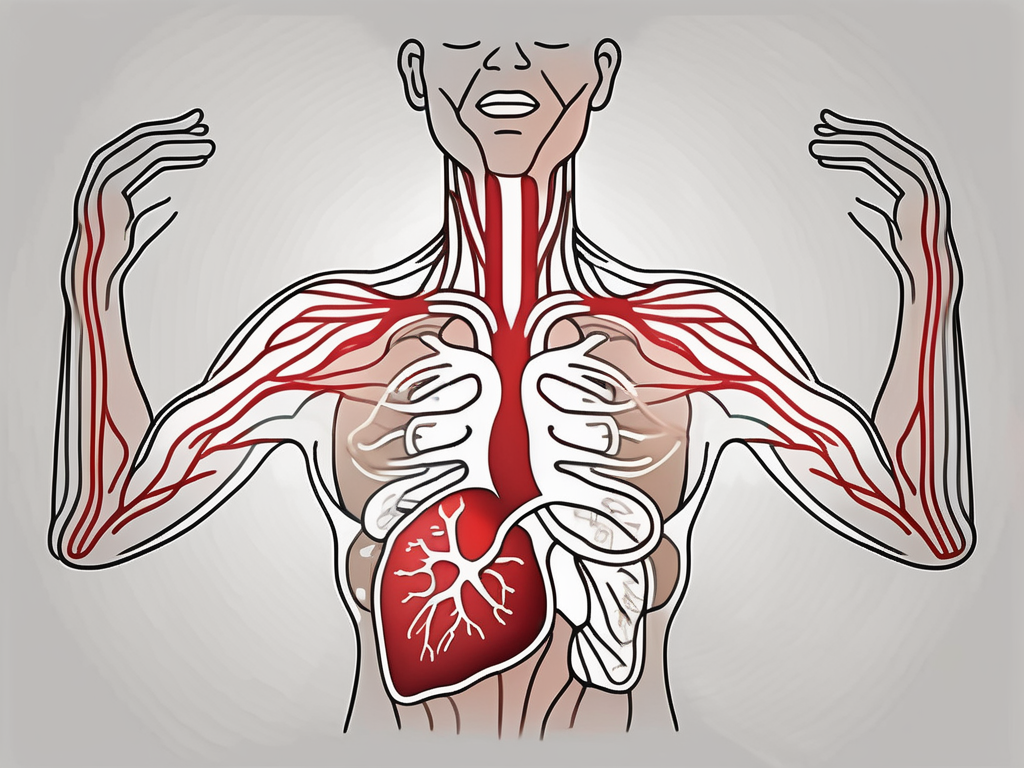
Before we can comprehend the connection, it is important to define vasovagal syncope. This condition occurs when there is an overreaction of the vagus nerve, which controls various bodily functions such as heart rate and blood pressure. This overreaction leads to a sudden drop in blood pressure and a decrease in heart rate, resulting in fainting. While it may seem alarming, vasovagal syncope is typically harmless and can be attributed to certain triggers.
Vasovagal syncope can be a perplexing phenomenon for those who experience it. The sudden loss of consciousness can be disorienting and concerning, but understanding the underlying physiology can provide some clarity.
The Physiology of Vasovagal Syncope
To understand the physiology of vasovagal syncope, we need to examine the autonomic nervous system. This system regulates vital bodily functions that we do not consciously control, such as breathing and digestion. Within this system, the vagus nerve plays a crucial role.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem to various organs, including the heart, lungs, and digestive system. When the vagus nerve becomes excessively stimulated, it causes a series of reactions that manifest as vasovagal syncope.
These reactions include a sudden decrease in heart rate, widening of blood vessels, and a drop in blood pressure. The body’s normal functioning is disrupted, leading to a temporary loss of consciousness. It is important to note that while vasovagal syncope may seem alarming, it is generally a protective mechanism of the body, ensuring that vital organs receive adequate blood flow during times of stress or injury.
Common Triggers of Vasovagal Syncope
Understanding the triggers of vasovagal syncope is essential for individuals who experience this condition. By identifying and managing these triggers, individuals can better prevent episodes of fainting and maintain their overall well-being.
One common trigger of vasovagal syncope is prolonged standing. When a person stands for an extended period, blood can pool in the lower extremities, leading to a decrease in blood flow to the brain. This reduced blood flow can trigger a vasovagal response, resulting in fainting.
Intense emotional stress can also provoke vasovagal syncope. The body’s response to stress involves the release of stress hormones, which can affect the autonomic nervous system. This hormonal cascade can lead to an overstimulation of the vagus nerve, triggering a vasovagal episode.
Pain, whether acute or chronic, can be another trigger for vasovagal syncope. The body’s response to pain involves a complex interaction between the nervous system and various physiological processes. In some cases, the body’s pain response can activate the vagus nerve, leading to a vasovagal reaction and subsequent loss of consciousness.
Dehydration is another factor that can contribute to vasovagal syncope. When the body lacks sufficient fluid, blood volume decreases, which can result in low blood pressure. This drop in blood pressure can trigger a vasovagal response, causing fainting.
Hot or crowded environments can also be potential triggers for vasovagal syncope. In these situations, the body may struggle to regulate its temperature, leading to increased sweating and a potential drop in blood pressure. Additionally, being in a crowded space can induce feelings of anxiety or claustrophobia, which can activate the vagus nerve and trigger a vasovagal episode.
It is important for individuals who experience vasovagal syncope to identify their specific triggers and take appropriate measures to manage them. This may involve making lifestyle changes, such as avoiding prolonged standing or staying hydrated, and implementing stress-reduction techniques to mitigate the risk of fainting episodes.
Exploring Anxiety Disorders
Anxiety disorders encompass a range of conditions characterized by excessive and persistent feelings of fear and worry. These disorders can have a profound impact on an individual’s daily life, relationships, and overall well-being. Understanding the different types of anxiety disorders is essential for accurate diagnosis and effective treatment. In this article, we will focus on two common types: generalized anxiety disorder (GAD) and panic disorder.
Generalized Anxiety Disorder and its Symptoms
Generalized anxiety disorder is a chronic condition where individuals experience excessive worry and anxiety about everyday life events. It is not uncommon for people with GAD to constantly anticipate disaster and be overly concerned about their health, work, or relationships. This constant state of worry can be exhausting and interfere with their ability to function normally.
Common symptoms of GAD include restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbances. Individuals with GAD may find it challenging to relax and often feel on edge or easily startled. They may also experience physical symptoms such as headaches, stomachaches, or other gastrointestinal issues.
It is important to note that anxiety disorders are diagnosable conditions and should be assessed by a healthcare professional. A thorough evaluation by a mental health specialist is necessary to determine if an individual meets the criteria for GAD and to rule out other possible causes of their symptoms.
Panic Disorder and its Manifestations
Panic disorder is another type of anxiety disorder that is characterized by recurrent panic attacks. These attacks are intense episodes of fear and discomfort that can manifest with symptoms such as heart palpitations, chest pain, shortness of breath, dizziness, and a sense of impending doom. Panic attacks can be terrifying and may lead individuals to believe that they are experiencing a heart attack or going crazy.
People with panic disorder often live in fear of having another panic attack and may avoid situations or places where they have previously experienced an attack. This avoidance behavior can significantly impact their daily life, limiting their ability to engage in normal activities or socialize with others.
Seeking appropriate medical attention for accurate diagnosis and treatment is crucial for individuals with panic disorder. A mental health professional can help individuals understand their symptoms, develop coping strategies, and explore treatment options such as therapy and medication.
In conclusion, anxiety disorders, such as generalized anxiety disorder and panic disorder, are complex conditions that can have a profound impact on individuals’ lives. Recognizing the symptoms and seeking professional help is the first step towards managing and overcoming these disorders. With the right support and treatment, individuals can regain control of their lives and experience a greater sense of well-being.
The Intersection of Vasovagal Syncope and Anxiety
Now that we have examined the individual components, let us explore the intersection between vasovagal syncope and anxiety. Both conditions share the common thread of triggering the autonomic nervous system, leading to physiological responses that can result in fainting or panic attacks.
The Role of Stress and Fear in Vasovagal Syncope
Stress and fear play significant roles in the occurrence of vasovagal syncope. When individuals experience high levels of stress or fear, the body initiates the “fight or flight” response, which activates the autonomic nervous system. This response prepares the body to either confront the perceived threat or flee from it. In the case of vasovagal syncope, the body’s response can be overly intense, leading to a sudden drop in blood pressure and a subsequent loss of consciousness.
It is important to note that not all individuals will experience vasovagal syncope in response to stress or fear, and the severity of these reactions can vary. Factors such as genetic predisposition, underlying medical conditions, and individual coping mechanisms can influence the likelihood and intensity of vasovagal syncope episodes.
Moreover, the relationship between stress and vasovagal syncope is complex. While stress can act as a trigger for some individuals, the experience of vasovagal syncope itself can also be a significant source of stress. This creates a potential feedback loop, where stress triggers syncope episodes, and the episodes, in turn, increase stress levels.
Anxiety as a Precursor to Vasovagal Syncope
On the other hand, anxiety disorders, such as Generalized Anxiety Disorder (GAD) and panic disorder, can act as precursors to vasovagal syncope. The constant worry and fear individuals experience can heighten their sensitivity to certain triggers, potentially leading to vasovagal syncope episodes.
Individuals with anxiety disorders often have an overactive amygdala, which is the brain’s fear center. This hyperactivity can cause exaggerated responses to perceived threats, activating the autonomic nervous system and triggering physiological changes. In the context of vasovagal syncope, this can result in a sudden drop in blood pressure and subsequent loss of consciousness.
While the exact mechanisms behind the connection between anxiety and vasovagal syncope are still being studied, it is crucial for individuals with anxiety disorders to be aware of this possibility and take steps to manage their anxiety effectively. Treatment options such as therapy, medication, and stress-reducing techniques can help individuals with anxiety disorders reduce the frequency and severity of vasovagal syncope episodes.
Furthermore, it is worth noting that the relationship between anxiety and vasovagal syncope is not unidirectional. The experience of vasovagal syncope itself can also contribute to the development or exacerbation of anxiety. The fear of fainting or experiencing a panic attack in public settings can lead to anticipatory anxiety, causing individuals to avoid certain situations or develop phobias.
In conclusion, the intersection of vasovagal syncope and anxiety is a complex and multifaceted phenomenon. Stress and fear can trigger vasovagal syncope episodes, while anxiety disorders can act as precursors to syncope. Understanding the relationship between these two conditions is crucial for effective management and treatment. By addressing both the physiological and psychological aspects, individuals can work towards minimizing the impact of vasovagal syncope and anxiety on their daily lives.
Medical Research on the Connection
Recent medical research has shed light on the connection between vasovagal syncope and anxiety. While more studies are needed to fully understand the shared mechanisms, some significant findings have emerged.
Vasovagal syncope, also known as neurocardiogenic syncope, is a condition characterized by a sudden loss of consciousness due to a drop in blood pressure and a decrease in heart rate. It is often triggered by certain stimuli, such as emotional distress, pain, or the sight of blood. Anxiety, on the other hand, is a mental health disorder characterized by excessive worry, fear, and apprehension.
Recent Findings on the Vasovagal-Anxiety Link
A study conducted by researchers at a leading medical institution found that individuals with anxiety disorders are more likely to experience vasovagal syncope compared to those without anxiety. The study involved a large sample size and rigorous methodology, making the findings highly reliable.
Interestingly, the study also revealed that individuals who experienced both vasovagal syncope and anxiety had more severe symptoms and a higher frequency of syncope episodes. This suggests that anxiety may exacerbate the occurrence and severity of vasovagal syncope.
Furthermore, the study highlighted the importance of addressing anxiety symptoms as a part of the treatment plan for individuals with vasovagal syncope. By managing anxiety through therapy, medication, or a combination of both, healthcare providers can potentially reduce the frequency and intensity of syncope episodes.
It is essential to consult with a healthcare provider to discuss individual cases and receive appropriate guidance. Each person’s experience with vasovagal syncope and anxiety is unique, and a personalized treatment approach is necessary for optimal management.
Theories on the Shared Biological Mechanisms
Scientists theorize that there are shared biological mechanisms underlying the link between vasovagal syncope and anxiety. These mechanisms involve the autonomic nervous system’s dysregulation, neurotransmitter imbalances, and abnormal responses to stressors.
The autonomic nervous system plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, and stress response. In individuals with both vasovagal syncope and anxiety, the autonomic nervous system may be dysregulated, leading to an increased susceptibility to syncope episodes and heightened anxiety symptoms.
Neurotransmitters, such as serotonin and norepinephrine, are chemical messengers in the brain that play a role in mood regulation and stress response. Imbalances in these neurotransmitters have been implicated in both vasovagal syncope and anxiety disorders. Further research is needed to elucidate the specific neurotransmitter imbalances and their impact on the development and progression of these conditions.
Abnormal responses to stressors, such as an exaggerated fight-or-flight response, may also contribute to the link between vasovagal syncope and anxiety. When faced with stress or anxiety-provoking situations, individuals with both conditions may experience an overactivation of the sympathetic nervous system, leading to a cascade of physiological changes that can trigger syncope episodes.
Further research is crucial to expanding our understanding of these shared biological mechanisms and developing targeted treatments for individuals who experience both vasovagal syncope and anxiety. By unraveling the intricate connections between these conditions, healthcare providers can provide more effective interventions and improve the quality of life for affected individuals.
Treatment Approaches for Vasovagal Syncope and Anxiety
When it comes to managing vasovagal syncope and anxiety, a multimodal treatment approach is often recommended. It is paramount to consult with a healthcare professional to determine the best course of action tailored to individual needs.
Lifestyle Changes and Coping Strategies
For individuals experiencing vasovagal syncope and anxiety, making certain lifestyle changes can be beneficial. These changes may include prioritizing regular exercise, maintaining a balanced diet, staying hydrated, practicing stress-reducing techniques such as mindfulness and relaxation exercises, and avoiding triggers that may lead to episodes. Additionally, developing coping strategies, such as deep breathing techniques or distraction methods, can be helpful in managing anxiety symptoms and reducing the likelihood of vasovagal syncope episodes.
Medication and Therapy Options
In some cases, healthcare providers may recommend medication or therapy for individuals with vasovagal syncope and anxiety. Medications, such as beta-blockers or selective serotonin reuptake inhibitors (SSRIs), may be prescribed to regulate heart rate, blood pressure, or manage anxiety symptoms. Cognitive-behavioral therapy (CBT), a type of psychotherapy, can also be beneficial in addressing anxiety, identifying triggers, and developing coping mechanisms. However, it is crucial to consult with a healthcare provider to determine the most appropriate treatment plan.
Living with Vasovagal Syncope and Anxiety
Living with vasovagal syncope and anxiety can present challenges, but there are strategies to help manage daily life and minimize triggers.
Managing Daily Life and Minimizing Triggers
To manage daily life with vasovagal syncope and anxiety, it is crucial to prioritize self-care and employ preventive measures. This may include ensuring adequate hydration and nutrition, maintaining regular sleep patterns, and avoiding triggering situations or environments. Using relaxation techniques, such as deep breathing exercises or mindfulness meditation, can also help reduce anxiety. Additionally, it is essential to establish open communication with friends, family, and healthcare providers, as their support can be invaluable in managing these conditions.
Seeking Support and Building Resilience
Living with vasovagal syncope and anxiety can be challenging, both physically and emotionally. It is important to seek the support of healthcare professionals who specialize in these conditions, as they can provide guidance, monitor progress, and adjust treatment plans as necessary. Additionally, joining support groups or connecting with others who face similar challenges can help individuals build resilience and share experiences. Remember, managing vasovagal syncope and anxiety is a journey that should be approached with patience and compassion.
Conclusion
Understanding the link between vasovagal syncope and anxiety is a complex endeavor, but it offers valuable insights into the intertwined nature of our physiology and mental health. While further research is needed to fully comprehend this connection, individuals who experience both vasovagal syncope and anxiety can take proactive steps to manage their conditions. By working closely with healthcare professionals, making necessary lifestyle changes, exploring treatment options, and seeking support, individuals can lead fulfilling lives and minimize the impact of these conditions on their overall well-being.







Leave a Reply