As medical professionals, it is crucial for us to have a comprehensive understanding of the vasovagal response to injections. This physiological reaction, although quite common, can be distressing for patients and may even lead to complications if not managed properly. In this article, we will delve into the causes, symptoms, and effective management strategies for the vasovagal response.
What is the Vasovagal Response?
The vasovagal response, also known as vasovagal syncope or neurocardiogenic syncope, refers to a sudden drop in blood pressure and heart rate that occurs in response to certain triggers. These triggers can range from physical stimuli to psychological factors. Understanding the physiology of this response is key to efficiently managing it and providing appropriate care for affected individuals.
The Physiology of the Vasovagal Response
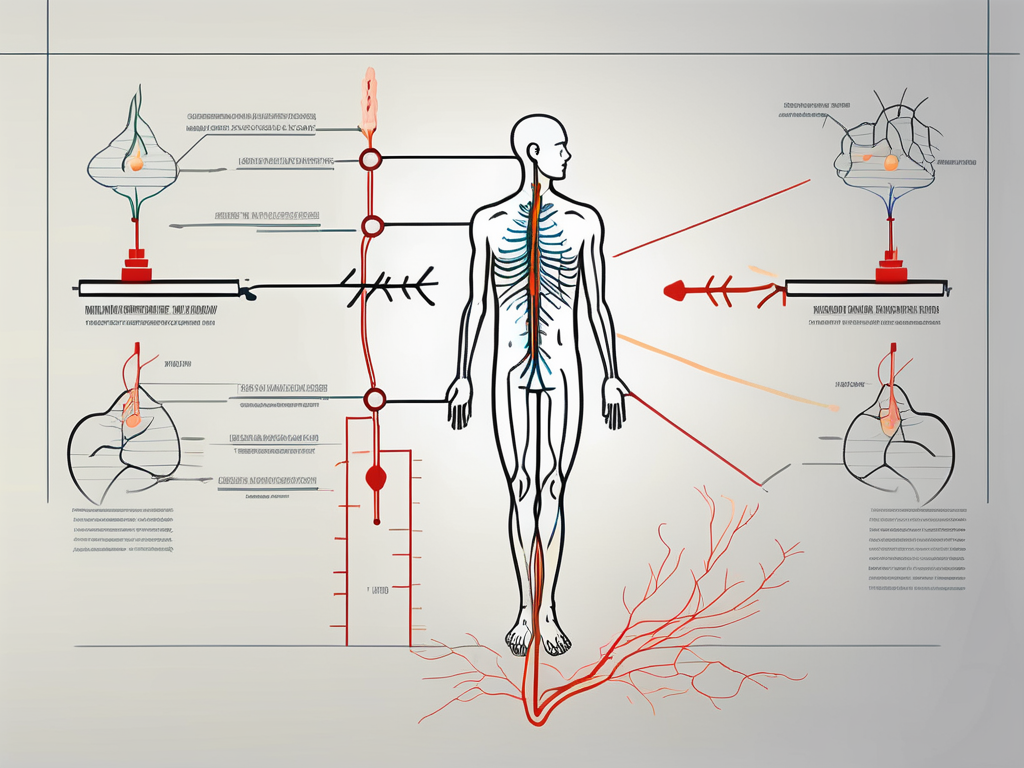
The vasovagal response involves a complex interplay between the nervous system and the cardiovascular system. It is primarily mediated by the vagus nerve, which is responsible for regulating various bodily functions, including heart rate and blood pressure. When triggered, the vagus nerve releases certain neurotransmitters that cause the blood vessels to dilate and the heart rate to slow down, thus leading to hypotension.
During a vasovagal response, the body’s natural defense mechanisms are activated. The brain perceives a potential threat or danger, whether real or imagined, and signals the vagus nerve to initiate the response. This can occur in situations such as seeing blood, experiencing pain, or feeling extreme emotional distress.
Once the vagus nerve is stimulated, it releases acetylcholine, a neurotransmitter that acts on the heart and blood vessels. Acetylcholine binds to specific receptors on the heart muscle cells, causing them to slow down the heart rate. At the same time, it also acts on the smooth muscle cells lining the blood vessels, causing them to relax and dilate. This combination of decreased heart rate and dilated blood vessels leads to a sudden drop in blood pressure.
Furthermore, the vasovagal response can also involve the release of other neurotransmitters, such as norepinephrine and serotonin, which play a role in modulating the response. These neurotransmitters can further contribute to the dilation of blood vessels and the overall hypotensive state.
Vasovagal Response vs. Normal Body Reaction
It is important to differentiate the vasovagal response from a normal body reaction to injections. While some degree of anxiety or discomfort is not uncommon during medical procedures, the vasovagal response goes beyond the typical stress response. This reaction is characterized by a sudden and significant drop in blood pressure, leading to dizziness, lightheadedness, and, in severe cases, loss of consciousness.
When a person experiences a vasovagal response, they may also exhibit other symptoms such as pale skin, sweating, nausea, and a feeling of warmth or coldness. These additional symptoms can vary from person to person and may depend on the specific trigger that initiated the response.
It is worth noting that the vasovagal response is not limited to medical settings. It can occur in various situations, such as standing for long periods, experiencing extreme fear or anxiety, or even during bowel movements. The triggers for a vasovagal response can be unique to each individual, and it is important to identify and avoid these triggers whenever possible.
In conclusion, the vasovagal response is a complex physiological reaction involving the vagus nerve, neurotransmitters, and the cardiovascular system. Understanding the intricacies of this response can help healthcare professionals provide appropriate care and management strategies for individuals who experience it. By recognizing the triggers and implementing preventive measures, the impact of the vasovagal response can be minimized, allowing individuals to lead a more comfortable and safe life.
Causes of Vasovagal Response to Injection
The vasovagal response, also known as vasovagal syncope, is a common physiological reaction that can occur during medical procedures involving injections. It is characterized by a sudden drop in blood pressure and heart rate, leading to dizziness, lightheadedness, and in some cases, fainting. Understanding the causes of this response is essential in effectively managing and preventing it.
Physical Triggers
Physical triggers play a significant role in inducing the vasovagal response. One of the most common physical triggers is pain. The sensation of pain during an injection can activate the body’s natural defense mechanisms, causing a sudden decrease in blood pressure and heart rate. Additionally, the fear of needles can also contribute to the vasovagal response. For some individuals, the mere sight of a needle can elicit a strong fear response, leading to a cascade of physiological changes that result in the vasovagal reaction. Moreover, the sight of blood can also act as a physical trigger. Some people have a heightened sensitivity to the sight of blood, which can stimulate the vasovagal response during injections.
Psychological Triggers
Psychological triggers can be just as influential in inducing the vasovagal response as physical triggers. Anxiety and fear related to medical procedures can have a profound impact on the body’s response to injections. The anticipation of an injection can trigger feelings of distress and anxiety, activating the body’s stress response. This, in turn, can lead to the vasovagal reaction. Phobias, specifically related to medical procedures or injections, can also play a role in triggering the vasovagal response. Individuals with a phobia of needles, for example, may experience heightened anxiety and fear, making them more susceptible to the vasovagal reaction.
It is important to note that the vasovagal response is a complex physiological reaction that can be influenced by a combination of physical and psychological factors. Each individual may have unique triggers that can induce this response, making it crucial to identify and address these triggers in order to effectively manage and prevent the vasovagal response during injections.
Recognizing the Symptoms of Vasovagal Response
Properly recognizing the symptoms of the vasovagal response is essential in providing timely care and preventing complications. These symptoms can be categorized into immediate and delayed manifestations.
The vasovagal response, also known as neurocardiogenic syncope, is a common cause of fainting. It occurs when there is a sudden drop in heart rate and blood pressure, leading to a temporary loss of consciousness. Understanding the symptoms associated with this response can help healthcare professionals and individuals identify it accurately.
Immediate Symptoms
Immediately following the vasovagal response, individuals may experience dizziness, lightheadedness, pale skin, nausea, and, in severe cases, loss of consciousness. These symptoms occur due to the body’s natural response to stress or certain triggers, such as the sight of blood, pain, or emotional distress.
Dizziness and lightheadedness are commonly reported symptoms during a vasovagal response. The sudden drop in blood pressure can cause inadequate blood flow to the brain, resulting in a feeling of lightheadedness or a spinning sensation. Some individuals may also experience blurred vision or tunnel vision, further contributing to the disorienting feeling.
Another visible sign of a vasovagal response is pale skin. When blood pressure drops, the body redirects blood flow away from the skin’s surface to vital organs, causing a paleness in complexion. This paleness is often noticeable in the face, but it can also affect other parts of the body.
Nausea is another common symptom experienced during a vasovagal response. The sudden shift in blood flow and the body’s response to stress can trigger the feeling of queasiness or an upset stomach. This symptom may be accompanied by cold sweats or clammy skin.
In severe cases, individuals may lose consciousness during a vasovagal response. This loss of consciousness is temporary and typically lasts for a few seconds to a minute. It occurs due to the brain not receiving enough oxygenated blood during the episode. It is important to differentiate these symptoms from other possible causes of fainting, such as cardiac issues, to ensure appropriate management.
Delayed Symptoms
In some cases, individuals may experience delayed symptoms following a vasovagal response. These can include fatigue, headaches, and general feelings of malaise. These symptoms may not occur immediately after the episode but can manifest within hours or even days.
After experiencing a vasovagal response, the body may feel fatigued and weak. This fatigue can be attributed to the stress and exertion the body went through during the episode. It is important for individuals to rest and allow their bodies to recover fully.
Headaches are another delayed symptom that some individuals may experience. The sudden drop in blood pressure and oxygen levels during the vasovagal response can trigger a headache. These headaches are usually mild to moderate in intensity and can be relieved with rest and hydration.
General feelings of malaise, such as a sense of unease or discomfort, may also be present after a vasovagal response. This can be due to the body’s reaction to the stress it experienced during the episode. It is crucial to monitor patients closely and address any concerns or discomfort they may have.
While delayed symptoms following a vasovagal response are generally not a cause for immediate medical attention, it is essential to inform healthcare professionals about any persistent or worsening symptoms. This will ensure appropriate follow-up care and management of the condition.
Management and Prevention of Vasovagal Response
Effective management and prevention strategies play a pivotal role in ensuring patient comfort and safety during injections. Medical professionals can employ various techniques to achieve this goal.
Vasovagal response, also known as vasovagal syncope, is a common physiological reaction that can occur during medical procedures such as injections. It is characterized by a sudden drop in heart rate and blood pressure, leading to a temporary loss of consciousness. While vasovagal response is generally harmless, it can cause distress for both patients and healthcare providers. Therefore, implementing strategies to manage and prevent this response is crucial.
Pre-Injection Strategies
Prior to performing an injection, it is vital to establish clear communication with the patient. This involves addressing any fears or concerns they may have, providing explanations about the procedure, and ensuring their comfort. Creating a supportive and empathetic environment can help alleviate anxiety and build trust between the patient and the healthcare provider.
Furthermore, distraction techniques can be employed to reduce the likelihood of a vasovagal response. Deep breathing exercises, for instance, can help calm the patient’s nervous system and promote relaxation. Engaging the patient in conversation about topics unrelated to the injection can also divert their attention away from the procedure, minimizing anxiety.
In addition to these techniques, some medical professionals may choose to use topical anesthetics or numbing creams to minimize the discomfort associated with injections. By reducing the physical sensation of the needle entering the skin, patients may experience less anxiety and a lower risk of vasovagal response.
Post-Injection Care
Following the injection, it is important to monitor the patient closely. This includes observing their vital signs, such as heart rate and blood pressure, to detect any signs of a vasovagal response. Prompt recognition of symptoms can facilitate timely intervention and prevent complications.
If a vasovagal response does occur, laying the patient down in a safe position and elevating their legs can help restore blood flow to the brain. This position, known as the Trendelenburg position, promotes venous return and counteracts the drop in blood pressure. Additionally, loosening any tight clothing around the patient’s neck or chest can further improve blood flow and alleviate symptoms.
Providing emotional support and reassurance is also crucial during and after a vasovagal response. Patients may feel embarrassed or anxious following an episode, and offering understanding and empathy can help alleviate any distress. Healthcare providers should take the time to explain what happened, reassure the patient that vasovagal responses are common and not indicative of a serious medical condition, and answer any questions or concerns the patient may have.
In conclusion, the management and prevention of vasovagal response during injections involve a combination of pre-injection strategies aimed at reducing anxiety and distraction, as well as post-injection care focused on monitoring and providing support. By implementing these techniques, healthcare professionals can enhance patient comfort and safety, ensuring a positive experience for both patients and providers.
The Role of Medical Professionals in Managing Vasovagal Response
Medical professionals have a critical role in managing and addressing the vasovagal response effectively. This encompasses patient education, communication, and emergency response when necessary.
The vasovagal response, also known as vasovagal syncope, is a common and often benign condition that occurs when there is a sudden drop in heart rate and blood pressure, leading to a temporary loss of consciousness. It can be triggered by various factors, including pain, fear, anxiety, or even the sight of blood. While it is generally not a cause for concern, it can be distressing for both patients and medical professionals.
Patient Education and Communication
Informing patients about the possibility of a vasovagal response is crucial in managing their expectations and reducing anxiety. By explaining that this reaction is relatively common and not necessarily indicative of a serious underlying condition, patients can approach injections with a sense of understanding and preparedness.
Medical professionals should take the time to educate patients about the physiological mechanisms involved in a vasovagal response. They can explain that the body’s autonomic nervous system, which controls involuntary functions like heart rate and blood pressure, can sometimes overreact to certain triggers, leading to a temporary disruption in blood flow to the brain.
Furthermore, medical professionals should emphasize the importance of seeking medical advice and evaluation if symptoms persist or worsen. While vasovagal responses are typically harmless, there may be cases where further investigation is necessary to rule out any underlying medical conditions.
Emergency Response to Severe Vasovagal Reactions
While less common, severe vasovagal reactions can occur and may require immediate medical attention. Medical professionals should be equipped to recognize the signs of a severe vasovagal response, such as prolonged loss of consciousness or difficulty breathing, and respond accordingly.
In such cases, prompt intervention is crucial to ensure the patient’s safety and well-being. Medical professionals may administer medication, such as intravenous fluids, to help stabilize the patient’s blood pressure and heart rate. They may also consider performing additional tests or evaluations to rule out any underlying causes for the severe vasovagal response.
If the situation warrants it, medical professionals may need to seek assistance from emergency medical services. This can ensure that the patient receives the appropriate care and attention in a timely manner, especially if the vasovagal response is accompanied by other concerning symptoms or if the patient’s condition does not improve with initial interventions.
In conclusion, medical professionals play a vital role in managing vasovagal responses. Through patient education and effective communication, they can help alleviate anxiety and ensure that patients are well-informed about the condition. In cases of severe vasovagal reactions, medical professionals must be prepared to respond promptly and appropriately to ensure the patient’s safety and well-being.
Living with a Proneness to Vasovagal Response
For individuals who are prone to experiencing the vasovagal response, certain lifestyle modifications and psychological support can significantly improve their quality of life and reduce the frequency of episodes.
Lifestyle Modifications
Implementing stress management techniques, such as regular exercise, meditation, or yoga, can help individuals cope with general anxiety and reduce the likelihood of a vasovagal response. Moreover, staying well-hydrated and ensuring an adequate intake of salt can contribute to maintaining stable blood pressure levels.
Psychological Support and Therapy
For individuals who experience significant emotional distress related to medical procedures, seeking psychological support or therapy can be beneficial. Cognitive-behavioral therapy and exposure therapy are commonly employed techniques that can aid in addressing the underlying fears or phobias associated with injections or medical settings.
In conclusion, understanding the vasovagal response to injection is fundamental in providing appropriate care for affected individuals. By familiarizing ourselves with the causes, recognizing the symptoms, and implementing effective management strategies, we can ensure a safe and comfortable experience for our patients. Remember to consult with a healthcare professional for personalized advice and guidance.







Leave a Reply