Vasovagal syncope, also known as neurocardiogenic syncope or vasovagal episode, is a common and sudden loss of consciousness due to a temporary drop in blood flow to the brain. This article aims to provide a comprehensive understanding of vasovagal syncope seizures, including their causes, symptoms, and treatment options. It is important to note that this article is not a substitute for medical advice, and individuals experiencing vasovagal syncope should consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
What is Vasovagal Syncope?
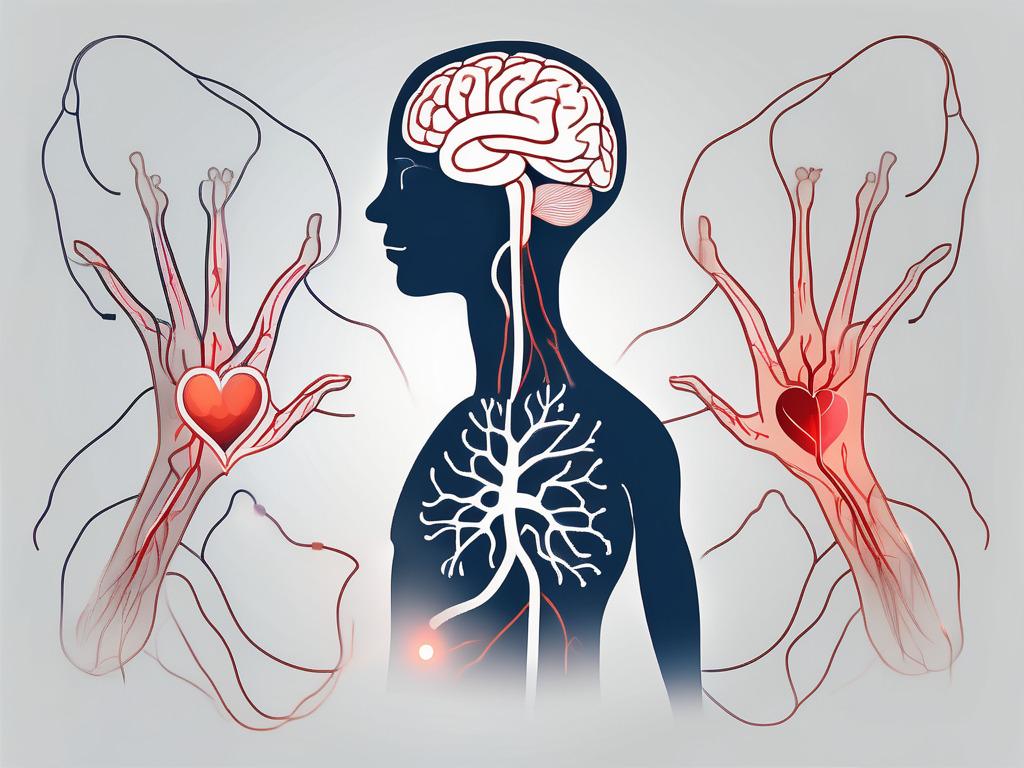
Vasovagal syncope is a condition characterized by a sudden and temporary loss of consciousness, often accompanied by a fall. It occurs when there is a malfunction in the autonomic nervous system, which regulates involuntary body functions such as heart rate, blood pressure, and digestion. In a vasovagal syncope episode, the autonomic nervous system overreacts to certain triggers, leading to a sudden drop in blood pressure and heart rate.
When a person experiences vasovagal syncope, it can be a frightening and disorienting experience. The sudden loss of consciousness can happen unexpectedly, making it important for individuals with this condition to be aware of their triggers and take necessary precautions to prevent episodes.
The Physiology of Vasovagal Syncope
The physiological mechanisms underlying vasovagal syncope involve the interplay between the parasympathetic and sympathetic divisions of the autonomic nervous system. During a vasovagal syncope episode, stimulation of the vagus nerve leads to the activation of the parasympathetic nervous system, causing blood vessels to widen and blood pressure to decrease. Additionally, the heart rate slows down, resulting in inadequate blood supply to the brain and subsequent loss of consciousness.
Understanding the physiology of vasovagal syncope helps medical professionals develop effective treatment plans for individuals with this condition. By targeting the underlying mechanisms, they can help manage symptoms and improve quality of life.
Common Triggers of Vasovagal Syncope
Vasovagal syncope can be triggered by various factors, which may vary from person to person. Some common triggers include:
- Prolonged standing or sitting
- Emotional stress or fear
- Pain or the sight of blood
- Dehydration
- Heat exposure
- Certain medications or medical procedures
Understanding the triggers of vasovagal syncope is crucial for individuals with this condition to prevent episodes. By avoiding or managing these triggers, they can reduce the frequency and severity of syncope episodes, leading to a better quality of life.
Prolonged standing or sitting can lead to blood pooling in the legs, which can trigger a vasovagal syncope episode. It is important for individuals who are prone to syncope to take regular breaks and move around to improve blood circulation.
Emotional stress or fear can also trigger vasovagal syncope. The body’s response to stress can cause the autonomic nervous system to overreact, leading to a sudden drop in blood pressure and heart rate. Learning stress management techniques and practicing relaxation exercises can help individuals with vasovagal syncope manage their symptoms.
Pain or the sight of blood can be powerful triggers for vasovagal syncope. The body’s response to pain or the sight of blood can activate the autonomic nervous system, leading to a sudden drop in blood pressure and loss of consciousness. Individuals who are prone to syncope should be cautious in situations where they may encounter these triggers and seek medical attention if necessary.
Dehydration can also contribute to vasovagal syncope. When the body is dehydrated, blood volume decreases, leading to a drop in blood pressure. It is important for individuals with vasovagal syncope to stay hydrated by drinking an adequate amount of fluids throughout the day.
Heat exposure can be a trigger for vasovagal syncope, especially in hot and humid environments. The body’s response to heat can cause blood vessels to dilate, leading to a drop in blood pressure. It is important for individuals with vasovagal syncope to avoid prolonged exposure to heat and stay in cool environments to prevent syncope episodes.
Certain medications or medical procedures can also trigger vasovagal syncope. It is important for individuals with this condition to inform their healthcare providers about their history of syncope to ensure that appropriate precautions are taken during medical procedures or when prescribing medications.
By understanding the common triggers of vasovagal syncope, individuals with this condition can take proactive steps to prevent episodes and improve their overall well-being.
Identifying the Symptoms of Vasovagal Syncope Seizures
The symptoms of vasovagal syncope seizures can vary in intensity and duration. It is important to recognize these symptoms to seek timely medical attention and avoid potential injuries. The symptoms can be categorized into physical symptoms and emotional/cognitive symptoms.
Physical Symptoms
During a vasovagal syncope episode, individuals may experience a range of physical symptoms. These symptoms can be alarming and may include:
- Lightheadedness or dizziness: One of the most common symptoms of vasovagal syncope seizures is a sudden feeling of lightheadedness or dizziness. This sensation can make it difficult to maintain balance and can be accompanied by a spinning sensation.
- Nausea or vomiting: Some individuals may experience nausea or even vomiting during a vasovagal syncope episode. This can be a result of the body’s response to the sudden drop in blood pressure.
- Pale skin: Another physical symptom that may occur during a vasovagal syncope seizure is a noticeable change in skin color. The skin may appear pale or even slightly bluish due to the reduced blood flow to the surface of the skin.
- Sweating: Excessive sweating is a common physical response during a vasovagal syncope episode. The body’s autonomic nervous system goes into overdrive, causing an increase in sweat production.
- Blurred vision: Blurred vision is a distressing symptom that can occur during a vasovagal syncope seizure. Individuals may experience a temporary loss of clear vision, making it difficult to see objects or read.
- Feeling hot or cold: During a vasovagal syncope episode, individuals may experience sudden changes in body temperature. Some may feel a sudden wave of heat, while others may feel a chill running through their body.
Emotional and Cognitive Symptoms
In addition to physical symptoms, vasovagal syncope seizures can also lead to emotional and cognitive changes. These symptoms can be equally distressing and may include:
- Anxiety or panic: It is not uncommon for individuals experiencing a vasovagal syncope seizure to feel a sense of anxiety or panic. The sudden onset of physical symptoms can be overwhelming and trigger a fear response.
- Confusion or disorientation: During a vasovagal syncope episode, individuals may experience confusion or a sense of disorientation. This can make it difficult to understand what is happening and may lead to a feeling of being disconnected from reality.
- Difficulty focusing or concentrating: The cognitive symptoms of vasovagal syncope seizures can also affect an individual’s ability to focus or concentrate. Tasks that require mental effort may become challenging, and thoughts may feel scattered or foggy.
It is important to note that the symptoms of vasovagal syncope seizures can vary from person to person. Some individuals may experience a combination of physical and emotional symptoms, while others may only experience a few. If you or someone you know is experiencing these symptoms, it is crucial to seek medical attention for proper diagnosis and treatment.
Causes and Risk Factors of Vasovagal Syncope Seizures
Vasovagal syncope seizures can be caused by various factors, including underlying health conditions and lifestyle/environmental factors. Understanding these causes and risk factors is essential in managing and preventing vasovagal syncope seizures.
Underlying Health Conditions
Several underlying health conditions can contribute to the development of vasovagal syncope seizures. These may include:
- Heart conditions, such as arrhythmias or structural abnormalities: When the heart’s electrical system malfunctions or there are structural issues, it can disrupt the normal blood flow and lead to syncope episodes.
- Blood pressure abnormalities: Both low blood pressure (hypotension) and high blood pressure (hypertension) can trigger vasovagal syncope seizures. Hypotension can cause inadequate blood flow to the brain, while hypertension can put excessive strain on the heart.
- Diabetes: People with diabetes may experience vasovagal syncope seizures due to fluctuations in blood sugar levels. Low blood sugar (hypoglycemia) can trigger syncope episodes.
- Anemia: When the body lacks enough healthy red blood cells to carry oxygen to the brain, it can result in syncope episodes.
- Neurological disorders: Certain neurological conditions, such as epilepsy or Parkinson’s disease, can increase the risk of vasovagal syncope seizures.
It is important for individuals experiencing vasovagal syncope to undergo a thorough medical evaluation to identify any underlying conditions that may be contributing to their symptoms. Proper diagnosis and treatment of these conditions can help manage and reduce the frequency of syncope episodes.
Lifestyle and Environmental Factors
Certain lifestyle and environmental factors can also increase the risk of vasovagal syncope seizures. These may include:
- Prolonged standing or sitting: Remaining in an upright position for an extended period can lead to blood pooling in the legs, causing a drop in blood pressure and triggering syncope episodes.
- Dehydration: Inadequate fluid intake can result in low blood volume, which can contribute to syncope episodes.
- Heat exposure: High temperatures can cause blood vessels to dilate, leading to a drop in blood pressure and potentially triggering syncope episodes.
- Stress or anxiety: Emotional stress or anxiety can activate the body’s fight-or-flight response, causing blood vessels to constrict and potentially leading to syncope episodes.
- Medications that affect blood pressure or heart rate: Certain medications, such as those used to treat high blood pressure or heart conditions, can affect blood pressure or heart rate regulation, increasing the risk of syncope episodes.
Identifying and addressing these lifestyle and environmental factors can play a crucial role in managing and preventing vasovagal syncope seizures. Lifestyle modifications, such as staying hydrated, avoiding prolonged periods of standing, and managing stress levels, can help reduce the frequency of syncope episodes.
Diagnostic Procedures for Vasovagal Syncope Seizures
Diagnosing vasovagal syncope seizures involves a careful evaluation of medical history, physical examination, and specialized tests and procedures.
When it comes to diagnosing vasovagal syncope seizures, healthcare professionals leave no stone unturned. They embark on a comprehensive journey, starting with a thorough exploration of the individual’s medical history. This includes delving into the depths of their symptoms, triggers, and any underlying health conditions that may be lurking beneath the surface.
But that’s not all. A meticulous physical examination is also an integral part of the diagnostic process. Healthcare professionals roll up their sleeves and get to work, meticulously checking blood pressure and heart rate. They keep their eyes peeled for any abnormalities or signs of other conditions that may be masquerading as vasovagal syncope seizures.
Specialized Tests and Procedures
While medical history and physical examination provide a solid foundation, specialized tests and procedures are often necessary to unearth the underlying causes and triggers of vasovagal syncope seizures. These tests are like detectives, gathering clues and piecing together the puzzle of the individual’s condition.
One of the key players in this diagnostic journey is the electrocardiogram (ECG). This test is like a window into the heart, allowing healthcare professionals to assess heart rhythm and electrical activity. It’s a vital tool that can reveal any irregularities or abnormalities that may be contributing to vasovagal syncope seizures.
But the heart isn’t the only star of the show. The echocardiogram also takes center stage. This test goes beyond the surface, delving deep into the structure and function of the heart. It provides a detailed evaluation, leaving no stone unturned in the quest for answers.
For some individuals, the tilt table test becomes a pivotal moment in their diagnostic journey. This test is designed to provoke and monitor symptoms, providing valuable insights into the mechanisms behind vasovagal syncope seizures. It’s like a rollercoaster ride, taking individuals on a journey that helps healthcare professionals understand their condition better.
But wait, there’s more. Blood tests also play a crucial role in the diagnostic process. These tests can check for underlying health conditions that may be contributing to vasovagal syncope seizures. They’re like detectives, searching for any hidden culprits that may be lurking in the shadows.
As healthcare professionals piece together the results of these specialized tests and procedures, a clearer picture of the individual’s condition begins to emerge. This newfound understanding is like a guiding light, leading the way towards an accurate diagnosis and effective treatment planning.
Treatment Options for Vasovagal Syncope Seizures
The treatment of vasovagal syncope seizures aims to reduce the frequency and severity of episodes, as well as manage any underlying health conditions contributing to the symptoms. The treatment plan may involve a combination of medications, therapies, surgical interventions, and lifestyle modifications.
Medications and Therapies
Depending on the individual’s specific case, healthcare professionals may prescribe medications or recommend therapies to manage vasovagal syncope seizures. Medications such as beta-blockers or anticholinergic drugs can help regulate heart rate and blood pressure. These medications work by blocking certain receptors in the body, which can help prevent the sudden drop in blood pressure and subsequent loss of consciousness.
In addition to medications, therapists may suggest techniques to help individuals recognize and manage early symptoms of vasovagal syncope. These techniques can include deep breathing exercises or muscle tensing, which can help increase blood flow to the brain and prevent fainting. Therapists may also provide education and counseling to help individuals cope with the emotional and psychological impact of living with vasovagal syncope seizures.
Surgical Interventions
In certain cases, surgical interventions may be considered to address underlying causes contributing to vasovagal syncope seizures. For example, pacemakers or implantable cardioverter-defibrillators (ICDs) might be recommended to ensure consistent heart rate and rhythm. These devices can monitor the heart’s electrical activity and deliver electrical shocks or pacing if an abnormal rhythm is detected.
Other surgical procedures, such as cardiac ablation, may be performed to correct any structural abnormalities in the heart that could be triggering the vasovagal syncope seizures. During cardiac ablation, a catheter is inserted into the heart and used to deliver radiofrequency energy to destroy or scar the tissue causing the abnormal electrical signals.
It is important to note that surgical interventions carry risks and require careful consideration and consultation with healthcare professionals. The decision to undergo surgery should be based on a thorough evaluation of the individual’s specific case and the potential benefits and risks of the procedure.
Lifestyle Modifications and Preventive Measures
Lifestyle modifications play a crucial role in managing vasovagal syncope seizures. Individuals are often advised to:
- Avoid triggers, such as prolonged standing or exposure to heat: These triggers can lead to a sudden drop in blood pressure and increase the risk of fainting. By avoiding these triggers, individuals can reduce the frequency of vasovagal syncope episodes.
- Maintain proper hydration: Dehydration can worsen symptoms of vasovagal syncope. It is important for individuals to stay adequately hydrated by drinking enough fluids throughout the day.
- Practice stress management techniques, such as meditation or yoga: Stress and anxiety can contribute to vasovagal syncope seizures. Engaging in stress-reducing activities can help individuals better manage their symptoms and reduce the likelihood of fainting.
- Gradually change positions, especially when transitioning from sitting to standing: Rapid changes in position can trigger vasovagal syncope episodes. Individuals are encouraged to take their time when transitioning from a seated to a standing position to allow their body to adjust to the change in blood flow.
By implementing these lifestyle modifications and preventive measures, individuals with vasovagal syncope seizures can significantly reduce the frequency and severity of episodes. It is important for individuals to work closely with their healthcare team to develop a comprehensive treatment plan that addresses their specific needs and goals.
Living with Vasovagal Syncope Seizures
Living with vasovagal syncope seizures may require individuals to make certain adjustments and adopt coping strategies to minimize the impact of the condition on their daily lives.
Coping Strategies and Support Systems
Coping strategies can help individuals manage vasovagal syncope seizures effectively. These strategies may include:
- Developing awareness of triggers and avoiding them
- Learning stress management techniques
- Carrying identification or medical alert information
- Building a support system by educating loved ones about the condition
In addition to individual coping strategies, support from healthcare professionals, support groups, and online communities can provide valuable guidance and emotional support during the journey of living with vasovagal syncope seizures.
Prognosis and Long-Term Management
The prognosis for individuals with vasovagal syncope seizures is generally good, with many experiencing a reduction in symptoms over time. However, the long-term management of the condition requires ongoing medical care, regular follow-ups, and adjustments to treatment plans as needed. It is essential for individuals to work closely with their healthcare team to ensure their symptoms are effectively managed and to address any changes or concerns that may arise.
Ultimately, understanding the causes, symptoms, and treatment options for vasovagal syncope seizures is vital in effectively managing this condition. It is important for individuals experiencing vasovagal syncope to seek medical attention for proper diagnosis and to work collaboratively with healthcare professionals to develop a personalized treatment plan that addresses their specific needs and circumstances.





Leave a Reply