Vasovagal Exercise: A Comprehensive Guide to Managing Symptoms
Vasovagal syncope is a condition that affects many individuals, causing a sudden loss of consciousness triggered by certain stimuli. If you have been diagnosed with vasovagal syncope or experience frequent episodes of fainting, incorporating exercise into your routine can play a crucial role in managing symptoms and improving your overall quality of life. In this comprehensive guide, we will explore the physiology behind vasovagal syncope, the connection between physical activity and syncope, recommended exercises, creating a personalized exercise plan, safety measures during exercise, the impact of lifestyle changes, medical treatments and interventions, as well as coping strategies and support.
Understanding Vasovagal Syncope
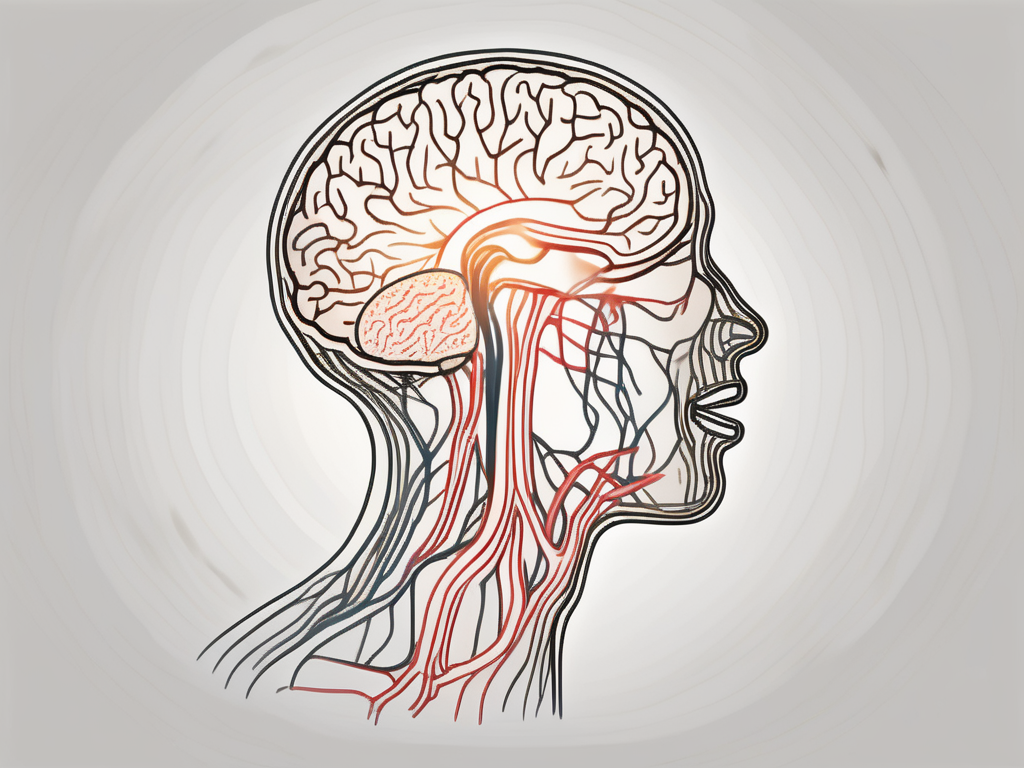
Vasovagal syncope is a common form of fainting, primarily caused by a sudden drop in blood pressure and heart rate due to the stimulation of the vagus nerve. This stimulation typically occurs in response to emotional distress, pain, or specific triggers, such as standing for prolonged periods or sudden changes in body position.
The Physiology Behind Vasovagal Syncope
To understand how exercise can help manage vasovagal syncope, it is essential to delve into the physiology of this condition. The vagus nerve, responsible for regulating heart rate and blood pressure, can become overly sensitive in individuals prone to vasovagal syncope. This heightened sensitivity prompts the body to react with a drop in blood pressure and heart rate, leading to loss of consciousness.
When the vagus nerve is stimulated, it releases a neurotransmitter called acetylcholine. Acetylcholine acts as a messenger, transmitting signals between nerve cells. In the case of vasovagal syncope, the release of acetylcholine leads to the dilation of blood vessels and a decrease in heart rate. This combination results in reduced blood flow to the brain, causing fainting.
Furthermore, the vagus nerve is intricately connected to the parasympathetic nervous system, which is responsible for the body’s “rest and digest” response. When the vagus nerve is activated, it sends signals to slow down the heart rate and relax the blood vessels, promoting a state of relaxation. However, in individuals with vasovagal syncope, this response becomes exaggerated, leading to fainting episodes.
Common Triggers of Vasovagal Syncope
Vasovagal syncope triggers vary from person to person. Some common triggers include prolonged standing, intense emotions, pain, and certain medical procedures such as blood draws or injections. Identifying your specific triggers can help you to manage and reduce the frequency of vasovagal episodes.
When it comes to prolonged standing, the blood pools in the lower extremities, leading to a decrease in blood flow to the brain. This reduction in blood flow can trigger the vagus nerve, causing a vasovagal response. Similarly, intense emotions, such as fear, anxiety, or even excitement, can stimulate the vagus nerve and result in syncope.
Pain is another significant trigger for vasovagal syncope. The body’s response to pain involves the release of endorphins, which can activate the vagus nerve and lead to a drop in blood pressure and heart rate. Additionally, certain medical procedures that involve needle insertions, like blood draws or injections, can stimulate the vagus nerve and trigger a vasovagal response.
It is important to note that while these triggers are common, they may not affect everyone with vasovagal syncope in the same way. Each individual’s response to triggers can vary, making it crucial to identify and manage personal triggers to minimize the risk of fainting episodes.
The Role of Exercise in Vasovagal Syncope Management
Exercise is an essential component in managing vasovagal syncope. Engaging in regular physical activity can help increase cardiovascular fitness, strengthen muscles, improve blood circulation, and enhance the body’s ability to handle stress. By incorporating exercise into your routine, you can potentially reduce the frequency and severity of vasovagal syncope episodes.
The Connection Between Physical Activity and Vasovagal Syncope
Regular physical activity has been shown to have a positive impact on individuals with vasovagal syncope. Exercise strengthens the cardiovascular system, making it more resistant to the triggers that can lead to fainting episodes. It increases heart rate variability, a key factor in maintaining proper blood pressure, and improves blood flow to the brain, reducing the risk of syncope.
Furthermore, exercise has been found to have a positive effect on overall mental health. It can help reduce anxiety and stress levels, which are known triggers for vasovagal syncope. By incorporating exercise into your routine, you not only improve your physical well-being but also enhance your mental well-being, leading to a more balanced and resilient body.
Research has also shown that exercise can improve the body’s autonomic nervous system function, which plays a crucial role in regulating blood pressure and heart rate. By engaging in regular physical activity, you can train your body to better respond to changes in blood pressure and heart rate, reducing the likelihood of vasovagal syncope episodes.
Recommended Exercises for Vasovagal Syncope
When incorporating exercise into your routine, it is important to choose activities that are suitable for your fitness level and health condition. Low-impact exercises such as walking, swimming, and cycling can be gentle on the body while providing the necessary cardiovascular benefits. These activities can be easily modified to suit individual needs and preferences.
In addition to cardiovascular exercises, it is also beneficial to include exercises that improve balance and stability. Yoga and tai chi, for example, focus on body awareness, flexibility, and core strength. These exercises can help prevent falls during potential fainting episodes, as they improve proprioception and enhance overall body control.
It is important to note that before starting any exercise program, individuals with vasovagal syncope should consult with their healthcare provider. They can provide personalized recommendations and guidance based on individual health status and specific triggers for syncope episodes.
In conclusion, exercise plays a crucial role in managing vasovagal syncope. By incorporating regular physical activity into your routine, you can strengthen your cardiovascular system, improve blood flow to the brain, and enhance your body’s ability to handle stress. Remember to choose exercises that are suitable for your fitness level and health condition, and always consult with your healthcare provider before starting any new exercise program.
Creating a Personalized Vasovagal Exercise Plan
Before starting any exercise program, it is crucial to assess your current fitness level and consult with your healthcare professional, who can provide guidance tailored to your individual needs. Together, you and your healthcare provider can determine an exercise plan that is safe and effective for managing vasovagal syncope.
Assessing Your Fitness Level
An initial step in creating a personalized exercise plan for vasovagal syncope is assessing your current fitness level. This evaluation will help determine the appropriate intensity and duration of exercise that is suitable for your unique situation. Working with a healthcare professional or a qualified exercise specialist can ensure accurate and personalized results.
During the fitness assessment, your healthcare provider will evaluate various aspects of your physical fitness, such as cardiovascular endurance, muscular strength, flexibility, and balance. They may conduct tests like the 6-minute walk test, which measures how far you can walk in 6 minutes, or the sit-and-reach test, which assesses your flexibility. These tests provide valuable information about your current fitness level and can help guide the development of your exercise plan.
Additionally, your healthcare provider may ask about your medical history and any previous experiences with vasovagal syncope. Understanding your medical background is essential in tailoring an exercise plan that takes into account any specific limitations or precautions you may need to consider.
Setting Realistic Exercise Goals
Once your fitness level has been assessed, it is essential to set realistic exercise goals. Start with small, attainable targets and gradually increase intensity and duration as your fitness improves. Keep in mind that each individual’s exercise tolerance may vary, so listen to your body and adjust accordingly.
When setting exercise goals, it is important to consider both short-term and long-term objectives. Short-term goals can be achieved within a few weeks or months and may include increasing the duration of your exercise sessions or improving your cardiovascular endurance. Long-term goals, on the other hand, may take several months or even years to accomplish and can include milestones like participating in a charity walk or completing a specific fitness challenge.
Working closely with your healthcare provider, you can establish realistic exercise goals that align with your overall health and wellness objectives. They can provide guidance on the appropriate frequency, intensity, and duration of exercise that will help you achieve your goals while managing vasovagal syncope effectively.
Safety Measures During Exercise
While exercise is generally beneficial, it is crucial to take certain safety measures to prevent injury or exacerbation of symptoms during physical activity.
Regular physical activity is essential for maintaining good health and well-being. It helps to strengthen muscles, improve cardiovascular health, and boost mood. However, it is important to approach exercise with caution and be mindful of your body’s limitations.
Here are some additional safety measures to consider:
Recognizing Warning Signs During Exercise
During exercise, it is essential to be aware of warning signs that could indicate impending syncope. These signs may include dizziness, lightheadedness, blurred vision, or palpitations. If you experience any of these symptoms during exercise, it is advisable to stop, rest, and consult a healthcare professional for guidance.
Furthermore, it is crucial to listen to your body and not push yourself beyond your limits. Overexertion can lead to injuries or other health complications. It is always better to start slowly and gradually increase the intensity and duration of your workouts.
What to Do in Case of a Vasovagal Episode During Exercise
If you experience a vasovagal episode while exercising, it is important to have a plan in place. Stop the activity immediately and, if possible, lie down with your legs elevated to increase blood flow to the brain. If you are unable to lie down, try to find a stable, seated position. Once the episode has passed, take your time to recover fully before resuming any physical activity.
It is worth mentioning that staying hydrated is crucial during exercise. Dehydration can increase the risk of vasovagal episodes and other complications. Make sure to drink plenty of water before, during, and after your workout sessions.
In addition, it is recommended to warm up before starting any intense exercise. A proper warm-up routine helps to prepare your muscles and joints for the physical demands of the workout, reducing the risk of strains or sprains.
Lastly, wearing appropriate clothing and footwear is essential for safety during exercise. Choose comfortable, breathable fabrics that allow for freedom of movement. Invest in well-fitting athletic shoes that provide adequate support and cushioning for your feet.
Remember, safety should always be a top priority when engaging in physical activity. By taking these precautions and being mindful of your body’s signals, you can enjoy the benefits of exercise while minimizing the risk of injury or complications.
The Impact of Lifestyle Changes on Vasovagal Syncope
In addition to exercise, making certain lifestyle changes can help manage vasovagal syncope and reduce the frequency of fainting episodes.
Vasovagal syncope, also known as neurocardiogenic syncope, is a common condition characterized by a sudden drop in blood pressure, leading to a temporary loss of consciousness. It can be triggered by various factors, including emotional stress, prolonged standing, and even certain medications.
While medication and medical interventions are available for managing vasovagal syncope, lifestyle changes play a crucial role in preventing and reducing the frequency of fainting episodes. These changes include dietary considerations and maintaining adequate hydration.
Dietary Considerations for Vasovagal Syncope
Adopting a balanced diet that includes foods rich in vitamins, minerals, and electrolytes can help maintain stable blood sugar levels and prevent dehydration, both of which can contribute to syncope. It is important to consume a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats.
Specifically, incorporating foods that are high in potassium, such as bananas, avocados, and spinach, can be beneficial. Potassium plays a crucial role in maintaining proper heart function and blood pressure regulation. Additionally, consuming foods rich in magnesium, such as nuts, seeds, and dark chocolate, can help relax blood vessels and improve blood flow.
It is recommended to speak with a registered dietitian or healthcare provider to discuss a diet plan that suits your specific needs. They can provide personalized guidance and ensure that your dietary choices align with your overall health goals.
The Importance of Adequate Hydration
Ensuring proper hydration is crucial for individuals with vasovagal syncope. Dehydration can lower blood volume and increase the risk of fainting episodes. It is important to drink water regularly throughout the day and pay attention to fluid intake during and after exercise.
In addition to water, incorporating electrolyte-rich beverages, such as sports drinks or coconut water, can help replenish essential minerals lost through sweating. Electrolytes, including sodium, potassium, and magnesium, play a vital role in maintaining proper fluid balance and supporting nerve and muscle function.
It is important to note that individual fluid needs may vary depending on factors such as age, weight, activity level, and climate. Consulting with a healthcare professional can help determine the appropriate amount of fluids to consume daily.
Furthermore, it is advisable to limit the consumption of caffeine and alcohol, as they can contribute to dehydration and potentially trigger vasovagal syncope episodes.
By making these dietary and hydration considerations, individuals with vasovagal syncope can take proactive steps in managing their condition and reducing the frequency of fainting episodes. However, it is essential to consult with a healthcare professional for personalized advice and guidance.
Medical Treatments and Interventions for Vasovagal Syncope
Although exercise and lifestyle changes can be beneficial, some individuals may require additional medical treatments or interventions to manage vasovagal syncope. It is important to consult with a healthcare professional to discuss the available options.
Medications Used in Vasovagal Syncope Management
In some cases, healthcare professionals may prescribe medications to help manage the symptoms of vasovagal syncope. Medications can be used to regulate heart rate, blood pressure, or reduce the sensitivity of the vagus nerve. However, the decision to use medication should be made on an individual basis, considering the potential benefits and risks.
When to Seek Medical Help
If you are experiencing frequent episodes of vasovagal syncope, it is important to seek medical help. Your healthcare provider can perform a thorough evaluation, which may include tests such as an electrocardiogram (ECG) or a tilt-table test, to determine the underlying cause and develop an appropriate treatment plan.
Coping Strategies and Support for Vasovagal Syncope
Living with vasovagal syncope can be challenging both physically and emotionally. Seeking support and implementing coping strategies can greatly assist individuals in managing their condition.
Emotional Impact of Living with Vasovagal Syncope
Dealing with the emotional impact of vasovagal syncope is an important aspect of managing this condition. Feelings of anxiety, fear, or frustration can arise due to the uncertainty and unpredictability of fainting episodes. It is essential to seek emotional support from friends, family, or support groups and consider counseling if necessary.
Finding Support and Community
Connecting with others who are also living with vasovagal syncope can provide valuable support and understanding. Support groups, both in-person and online, can offer a sense of community and a forum to share experiences, coping strategies, and advice. Engaging with others who have similar experiences can help alleviate feelings of isolation and provide a strong support network.
In conclusion, managing vasovagal syncope requires a multifaceted approach that includes exercise, lifestyle changes, medical interventions where necessary, and emotional support. By understanding the physiology behind vasovagal syncope, recognizing common triggers, choosing suitable exercises, creating a personalized exercise plan, implementing safety measures, making lifestyle changes, exploring medical treatments, and seeking support, individuals can take control of their condition and improve their quality of life. Remember, always consult with a healthcare professional to develop an approach tailored to your specific needs.







Leave a Reply